A Lifelong Journey: Holistic Care for Women Through Pregnancy and Beyond
Understanding Comprehensive Pregnancy Care
Definition and Scope of Comprehensive Pregnancy Care
Comprehensive pregnancy care refers to a complete approach to managing the health and well-being of women from preconception through postpartum. This care involves medical assessments, screenings, education, and emotional support tailored to each stage of the pregnancy journey. It includes routine check-ups, prenatal testing, nutrition guidance, and mental health monitoring to optimize both maternal and fetal outcomes.
Importance of a Continuum from Preconception to Postpartum
The pregnancy care continuum begins before conception with health optimization and preconception counseling and continues through pregnancy and the postpartum period. This seamless care transition ensures early identification and management of risks such as gestational diabetes and hypertensive disorders. Postpartum care focuses on physical recovery, mental health support, infant care, and chronic disease management, aiming to improve long-term health for mother and child.
Role of Personalized and Evidence-Based Care
Personalized care respects the unique needs and preferences of each woman, adapting visit schedules, screening, and interventions accordingly. Evidence-based practices guide clinical decisions, such as appropriate prenatal vitamin use, vaccination, and risk assessments for pregnancy complications. This individualized approach supports shared decision-making, improves satisfaction, and enhances health outcomes.
Collaborative Healthcare Providers Including OB/GYNs and Midwives
Effective comprehensive pregnancy care involves collaboration among obstetrician-gynecologists, certified nurse midwives, family medicine physicians, and other health professionals. Integration of these providers ensures access to specialized services, from routine prenatal visits and high-risk pregnancy management to labor support and postpartum follow-up. Such teamwork fosters coordinated, culturally sensitive care aligned with the best standards in women's health.
Preconception and Early Prenatal Care: Foundations for Healthy Pregnancies

Preconception counseling and health optimization
Preconception care is critical for women planning pregnancy, aiming to optimize health before conception. This includes managing chronic conditions like diabetes and hypertension, addressing lifestyle factors, and discussing reproductive plans. Healthcare providers guide women through medication adjustments and recommend healthy habits to reduce pregnancy complications. See Interconception care for primary care providers and Call to Action on Maternal Health.
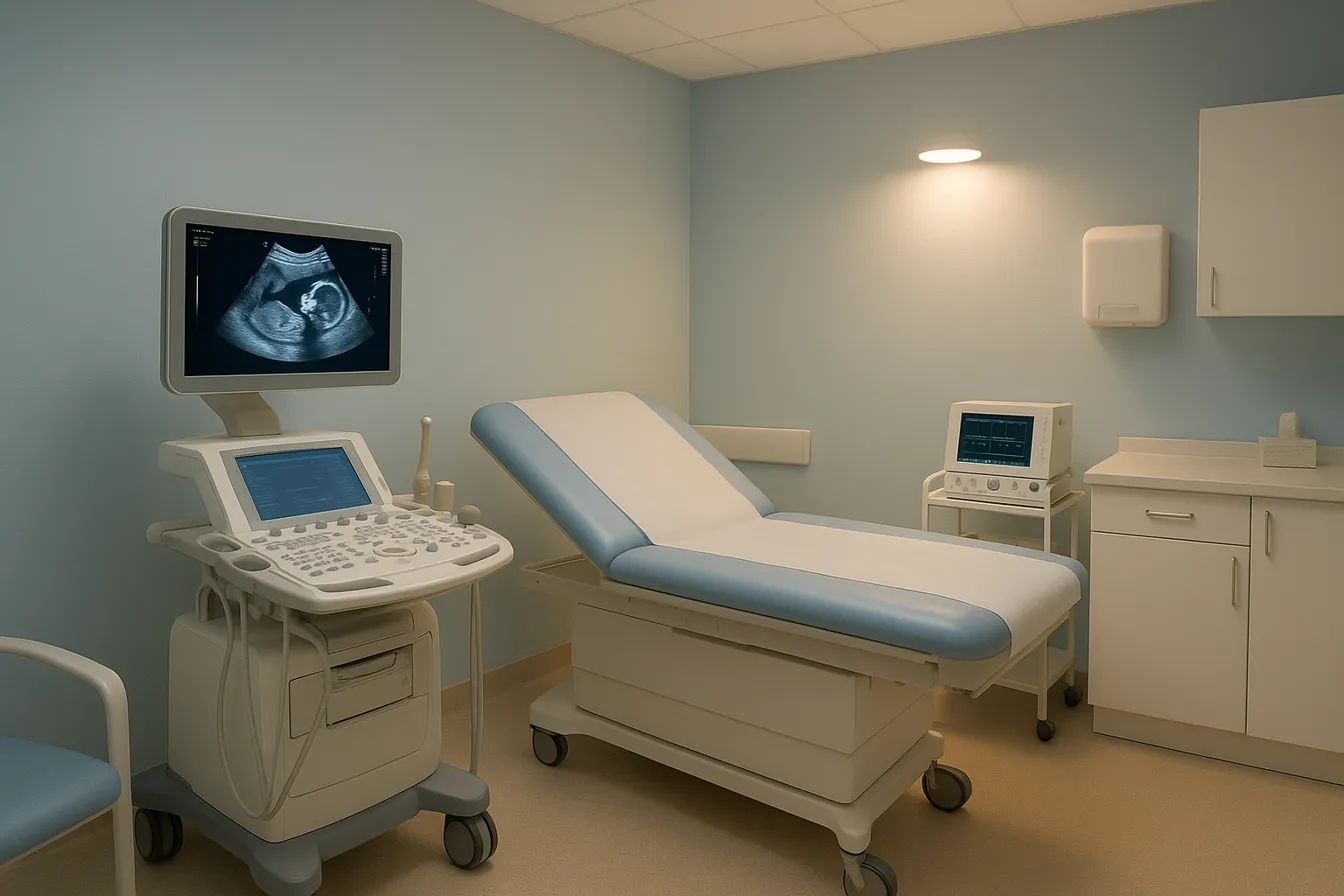
Early prenatal assessments and screenings within first trimester
Early prenatal care ideally begins within the first trimester with comprehensive assessments. These include a detailed medical history, physical exams, and important screenings such as blood type, infectious diseases, and genetic tests. Ultrasound evaluations confirm pregnancy dating, identify multiples, and detect anomalies. See Initial Antepartum Care and prenatal care basics.
Nutrition including folic acid supplementation
Adequate nutrition, especially folic acid supplementation of at least 400 micrograms daily, is essential to prevent neural tube defects and support fetal development. Pregnant individuals receive counseling on balanced diets enriched with vitamins and minerals important for maternal and fetal health. See Comprehensive Prenatal Care and prenatal care basics.
Identification of medical, social, and structural risk factors
Early visits also include assessments of Social determinants of prenatal care such as socioeconomic status, racism, and geographic barriers. Recognizing these factors helps tailor care plans to address disparities and improve access, particularly for marginalized populations. See Tailored prenatal care delivery and Call to Action on Maternal Health.
Incorporation of shared decision making and personalized care plans
Pregnant individuals are engaged in shared decision making to respect their preferences and individual circumstances. Personalized care plans are developed incorporating medical risks, social needs, and patient desires, ensuring tailored support throughout pregnancy. See Tailored prenatal care delivery.
Use of telemedicine and tailored prenatal visit schedules
Innovations like telemedicine and reduced in-person visits (6–10 instead of traditional 12–14 visits) have been adopted. These approaches maintain safety and convenience, improve access for those facing transportation challenges, and enhance patient satisfaction. See Tailored prenatal care delivery.
Addressing disparities in prenatal care access among marginalized populations
Due to social and structural barriers, marginalized communities often face delayed or incomplete prenatal care. Targeted strategies include early comprehensive needs assessments, culturally competent services, and referrals to community resources to close these gaps. See Tailored prenatal care delivery and Call to Action on Maternal Health.
Role of genetic counseling and management of preexisting conditions
Genetic counseling is integrated early to inform expectant parents about inheritance risks and available testing options. Women with preexisting medical conditions undergo specialized monitoring and interventions to mitigate risks and support healthy pregnancy outcomes. See Interconception care for primary care providers and prenatal care basics.
Innovative Prenatal Care Delivery: Tailored Models to Meet Diverse Needs

Traditional versus modern prenatal care models
Prenatal care in the United States has traditionally followed a standardized model involving scheduled, in-person visits aligned with pregnancy milestones. These visits aim to provide screening, medical care, and guidance for healthy pregnancies. However, this model has remained largely unchanged since the 1930s and may not address individual needs effectively.
Impact of COVID-19 on prenatal care, including telemedicine and remote monitoring
The COVID-19 pandemic accelerated the adoption of telemedicine in prenatal care and remote health monitoring in prenatal care. Video and audio consultations became common to reduce in-person visits, and pregnant individuals began self-monitoring vital parameters like blood pressure and weight with guidance from healthcare providers.
Group prenatal care benefits for psychosocial support
Group prenatal care benefits models, such as CenteringPregnancy, combine clinical assessments with education and group support. These have been shown to improve mental health outcomes, particularly reducing depressive symptoms for women facing psychosocial risks. Telehealth group programs have further increased accessibility and reduced social isolation.
Adjusting visit schedules based on risk and preferences
Evidence supports targeted visit schedules with fewer in-person appointments—around 6 to 10 visits instead of the traditional 12 to 14—without compromising maternal or neonatal outcomes. Adjusting prenatal care intensity according to individual risk factors and patient preferences enhances satisfaction and efficiency.
Use of home monitoring for vital signs
Home monitoring for pregnancy tools enable pregnant people to track blood pressure, weight, and other routine metrics from home, easing the burden of frequent clinic visits and increasing convenience while maintaining safety.
Community and health system interventions to address social determinants of health
Early comprehensive needs assessments help identify medical, social, and structural factors impacting pregnancy outcomes. Referrals to social workers, community resources, and targeted supports address disparities linked to racism, socioeconomic status, and geography within social determinants of prenatal care.
Ensuring equitable access to prenatal care through patient-centered approaches
Engaging pregnant individuals in shared decision-making and tailoring care plans respects their preferences and improves experiences. New care models emphasize patient-centered prenatal care, considering barriers like transportation and systemic bias to better serve marginalized populations.
Advanced Obstetric and Gynecologic Services in Queens, NY: A Woman-Led, Patient-Centered Approach

Description of Specialized OB/GYN Services Available in Queens
Queens offers a comprehensive range of Obstetrics and gynecology services in Queens, NY tailored to women of all ages, provided by experienced female physicians and multidisciplinary teams. These services include routine OB/GYN checkups, prenatal testing and care, reproductive endocrinology, fertility preservation, and state-of-the-art gynecologic treatment options.
Emphasis on Personalized Care by Female Physicians and Multidisciplinary Teams
Practices like Women for Women Obstetrics & Gynecology Queens in Queens feature female Board-certified OB/GYN providers who focus on individualized care plans that address each patient's unique medical and personal needs. This patient-centered women's health care approach is enhanced with collaboration among specialists for holistic management of health.
Management of High-Risk Pregnancies with Maternal-Fetal Medicine Collaboration
Queens hospitals partner closely with maternal fetal medicine specialists to manage complex pregnancies involving gestational diabetes, hypertensive disorders, or other complications. These collaborations ensure continuous monitoring, specialized testing, and tailored interventions.
Facilities Supporting Maternal and Neonatal Health Including NICU
Facilities across Queens include mother-baby unit at NewYork-Presbyterian Queens and Level III Neonatal Intensive Care Units (NICUs), such as those at Steven and Alexandra Cohen Children’s Medical Center and NewYork-Presbyterian Queens. These support units provide critical care for newborns requiring specialized attention.
Comprehensive Gynecologic Services Including Minimally Invasive Surgeries and Cancer Screening
Gynecologic care encompasses diagnosis and treatment for uterine fibroids, ovarian cysts, endometriosis, pelvic pain, and sexually transmitted infections. Minimally invasive surgeries such as laparoscopy and hysteroscopy help reduce recovery time and improve outcomes. Cancer screenings for cervical, breast, ovarian, and endometrial cancers are emphasized for prevention and early detection through Best OBGYN in Queens, NY.
Integration of Reproductive Endocrinology and Fertility Preservation
Fertility services in Queens include assessments of fertility, egg freezing, genetic testing, and reproductive endocrinology consultations. These services support family planning and assist women navigating fertility challenges or preparing for future pregnancies, as provided by Women’s health services at NYC Health + Hospitals/Queens.
Support Services Such as Abortion Care, Contraception Counseling, and Menopause Management
Queens health centers offer confidential abortion services up to 24 weeks with support including counseling and financial assistance through CHOICES Women's Medical Center. Comprehensive contraception counseling is provided to aid informed reproductive choices. Menopause treatment services are also addressed, offering hormonal and non-hormonal treatments tailored to women's health needs across life stages.
Tailored Postpartum Care: Supporting Physical, Emotional, and Long-Term Health

Why is postpartum care an ongoing and individualized process?
Postpartum care is best viewed as a continuous, personalized journey rather than a single medical visit. Each woman’s recovery and needs after childbirth differ, requiring Tailored Postpartum Services throughout the postpartum period to best support physical healing, emotional well-being, and long-term health.
What is the recommended schedule for postpartum visits?
An Initial Postpartum Contact with a healthcare provider should ideally occur within the first three weeks after birth to assess early recovery and address urgent concerns. This is followed by ongoing care based on individual needs, culminating in a Comprehensive Postpartum Visit no later than 12 weeks postpartum. This visit thoroughly evaluates Mood and Emotional Well-being Assessment, Infant Care and Feeding Guidance, Sexuality and Contraception Postpartum, sleep, Physical Recovery After Birth, Chronic Disease Management Postpartum, and Health Maintenance After Childbirth.
How do postpartum care visits assess mental health and support mothers?
Screening for Postpartum Depression and Anxiety using validated tools is a critical component. Early detection allows for timely referrals to appropriate mental health services, helping address common but serious conditions like Postpartum Depression and Anxiety. Mental health support is intertwined with physical recovery and infant care guidance.
How are women with pregnancy complications or chronic conditions supported postpartum?
Women who experienced complications such as Postpartum Care for Preterm Birth, Gestational Diabetes Postpartum Care, or Hypertensive Disorders and Postpartum Counseling require specialized counseling about their increased risk for lifelong cardiometabolic diseases. Those with Management of Chronic Health Conditions Postpartum like diabetes, hypertension, or mood disorders benefit from close, coordinated follow-up to manage ongoing health risks effectively.
What role does reproductive life planning play in postpartum care?
Discussions about reproductive goals, Contraception Options Postpartum, and Optimal Pregnancy Spacing are vital and should ideally begin during pregnancy and continue postpartum. Avoiding interpregnancy intervals shorter than six months is advised to reduce risks.
How does personalized postpartum care planning begin?
Developing a Personalized Postpartum Care Plan during pregnancy helps women identify their care team and clarify responsibilities for their ongoing health. This plan integrates medical follow-up, social support, and anticipates their unique recovery trajectory.
Why is policy advocacy important for postpartum care?
Policies that support postpartum care as an ongoing health process—including Reimbursement Policies for Postpartum Care for multiple visits—and advocate for Paid Parental Leave and Postpartum Outcomes greatly improve outcomes for mothers and infants. Supportive workplace and health policies create an environment that fosters recovery, bonding, and long-term health.
By embracing an individualized, continuous approach to postpartum care that addresses physical, emotional, and preventive health, healthcare providers can empower women through this transformative period and beyond.
Integrating Behavioral Health and Addressing Social Determinants Through Pregnancy and Postpartum

What Are the Prevalence and Risks of Perinatal Mental Health Conditions and Substance Use Disorders?
Perinatal Mental Health Disorders, Depression and Anxiety in Pregnancy and Postpartum, Substance Use Disorders in Reproductive-Aged Women, Tobacco, Alcohol, Marijuana, and Opioid Use During Pregnancy, Maternal Mortality and Morbidity Associated with Untreated Behavioral Health Conditions, Adverse Outcomes of Untreated Perinatal Mental Health and Substance Use Issues
How Are Screening Protocols and Assessment Tools Used?
Screening, Brief Interventions, and Treatment Referrals in Perinatal Behavioral Health, Universal Screening Tools for Perinatal Mental Health and Substance Use, Screening for Social Determinants of Health and Infectious Diseases in Pregnancy
What Are the Benefits of Integrated Behavioral Health Services?
Integration of Behavioral Health Services into Prenatal and Postpartum Care, Screening, Brief Interventions, and Treatment Referrals in Perinatal Behavioral Health
How Do Community Resources and Referral Systems Support Maternal Mental Health and Social Needs?
Call to Action on Maternal Health, Addressing Social Determinants of Maternal Health, Community Support for Women's Health
How Are Health Disparities Addressed in Behavioral Health Integration?
Reducing Maternal Health Disparities, Culturally Appropriate Healthcare for Women, Ensuring Equitable Access to Care
What Is the Role of Social Workers, Counseling, and Support Groups?
Social Support After Birth, Counseling for Pregnancy Complications, Emotional Support in Prenatal Care
How Do Social Determinants Impact Maternal Outcomes?
Social Determinants of Prenatal Care, Addressing Social Determinants of Maternal Health, Managing Social Needs in Pregnancy
Why Is Culturally Competent Care and Inclusive Education Important?
Culturally Competent Perinatal Care, Inclusive Health Education, Patient-Centered Prenatal Care
The integration of behavioral health and social determinants into prenatal and postpartum care is fundamental for improving maternal and infant health and reducing disparities across the United States.
The Critical Role of Interconception and Preventive Care in Women's Health
Managing Chronic Conditions Between Pregnancies
Effective interconception care for primary care providers focuses on controlling chronic conditions such as hypertension, diabetes, and obesity that increase pregnancy risks. Management includes timely follow-up to monitor blood pressure, blood sugar, and weight, aiming to optimize maternal and fetal outcomes in future pregnancies.
Preconception Assessment and Medication Optimization
Prior to conception, women should undergo comprehensive evaluation including medication review. Adjusting or switching to pregnancy-safe medications, such as replacing ACE inhibitors for hypertension, reduces risks to the developing fetus and prepares the body for a healthy pregnancy.
Screening and Counseling After Pregnancy Complications
Women with prior pregnancy complications like gestational diabetes or hypertensive disorders require targeted counseling and screening to assess recurrence risk and future cardiometabolic disease. Awareness and prevention strategies can mitigate long-term health consequences. See more at Hypertensive disorders and postpartum counseling.
Collaboration Between Primary Care and Specialists
Primary care providers play a pivotal role in ongoing interconception care by coordinating with obstetrics, endocrinology, and cardiology specialists. This team approach ensures comprehensive monitoring and management of medical conditions throughout the reproductive lifespan. For details, review Interconception care for primary care providers.
Prevention of Maternal Morbidity and Mortality
Long-term health maintenance, including screening for mood disorders and venous thromboembolism risk, alongside management of chronic diseases, is essential to reduce maternal morbidity and mortality beyond pregnancy. Learn more on Optimizing postpartum care.
Guidelines on Pregnancy Spacing
Health professionals recommend avoiding interpregnancy intervals shorter than six months due to increased risks such as preterm birth and adverse maternal health outcomes. Adequate spacing supports full recovery and risk reduction. Refer to Optimal pregnancy spacing.
Promoting Healthy Lifestyle and Preventive Screenings
Lifestyle interventions like balanced nutrition, exercise, smoking cessation, and weight management combined with regular preventive screenings contribute significantly to improved pregnancy outcomes and overall women's health during reproductive years. See healthy habits before pregnancy and prenatal care basics for more information.
Empowering Women Through Comprehensive and Compassionate Pregnancy Care
Comprehensive Care from Preconception to Postpartum
Pregnancy care is a continuous, multi-phase process beginning before conception and extending well into the postpartum period. It includes routine health assessments, nutrition and lifestyle counseling, prenatal screenings, and monitoring of both maternal and fetal health. Key components such as folic acid supplementation, blood pressure checks, ultrasounds, and gestational diabetes screening are essential to safeguard mother and baby.
Personalized and Culturally Sensitive Approach
Care is tailored to each woman's unique medical history, cultural background, and social circumstances. Early needs assessments and shared decision-making promote respect for individual preferences and enhance outcomes. This approach acknowledges disparities in access and embraces culturally appropriate practices to serve diverse populations effectively.
Integrated Support for Physical, Emotional, and Social Health
Holistic care integrates mental health screening—addressing postpartum depression and anxiety—with social support services. Collaboration among obstetricians, midwives, social workers, and community resources ensures women's comprehensive well-being throughout pregnancy and postpartum recovery.
Call to Action for Healthcare Systems and Policymakers
To empower women and families, healthcare systems must adopt ongoing postpartum care models, expand telemedicine, and provide equitable access. Policymakers play a vital role by endorsing reimbursement for continuous postnatal care and supporting paid parental leave, fostering better health outcomes and sustained wellness for mothers and children.




.png)