A Lifelong Journey: Holistic Care for Women Through Pregnancy and Beyond

Introduction to Fibroid Myomectomy
What is a myomectomy?
A myomectomy is a surgical procedure designed to remove uterine fibroids while preserving the uterus. It is distinct from hysterectomy, which removes the entire uterus, making myomectomy a preferred option for women who wish to retain their fertility and have future pregnancies.
Purpose of myomectomy
The primary goal of a myomectomy is to relieve symptoms caused by uterine fibroids such as heavy menstrual bleeding, pelvic pain, irregular bleeding, and pressure symptoms like difficulty emptying the bladder. By removing the fibroids, women often experience lighter, more regular periods and relief from discomfort.
Types of uterine fibroids
Fibroids, also known as leiomyomas, are benign growths of muscle and connective tissue that can form in different locations within or on the uterus. They are classified based on their position as:
- Intramural: within the uterine muscle wall
- Submucosal: just under the lining of the uterus
- Subserosal: on the outer surface of the uterus This classification helps determine the surgical approach and treatment strategy.
Who should consider myomectomy
Myomectomy is generally recommended for women who have symptomatic fibroids causing pain, heavy bleeding, or fertility issues and who want to keep their uterus intact. It is particularly suitable for women planning future pregnancies or those seeking to preserve uterine function. The type of myomectomy—whether abdominal, laparoscopic, robotic, or hysteroscopic—depends on factors such as fibroid size, number, and location, as well as the patient's overall health and fertility goals.
Preoperative Preparation for Myomectomy Surgery

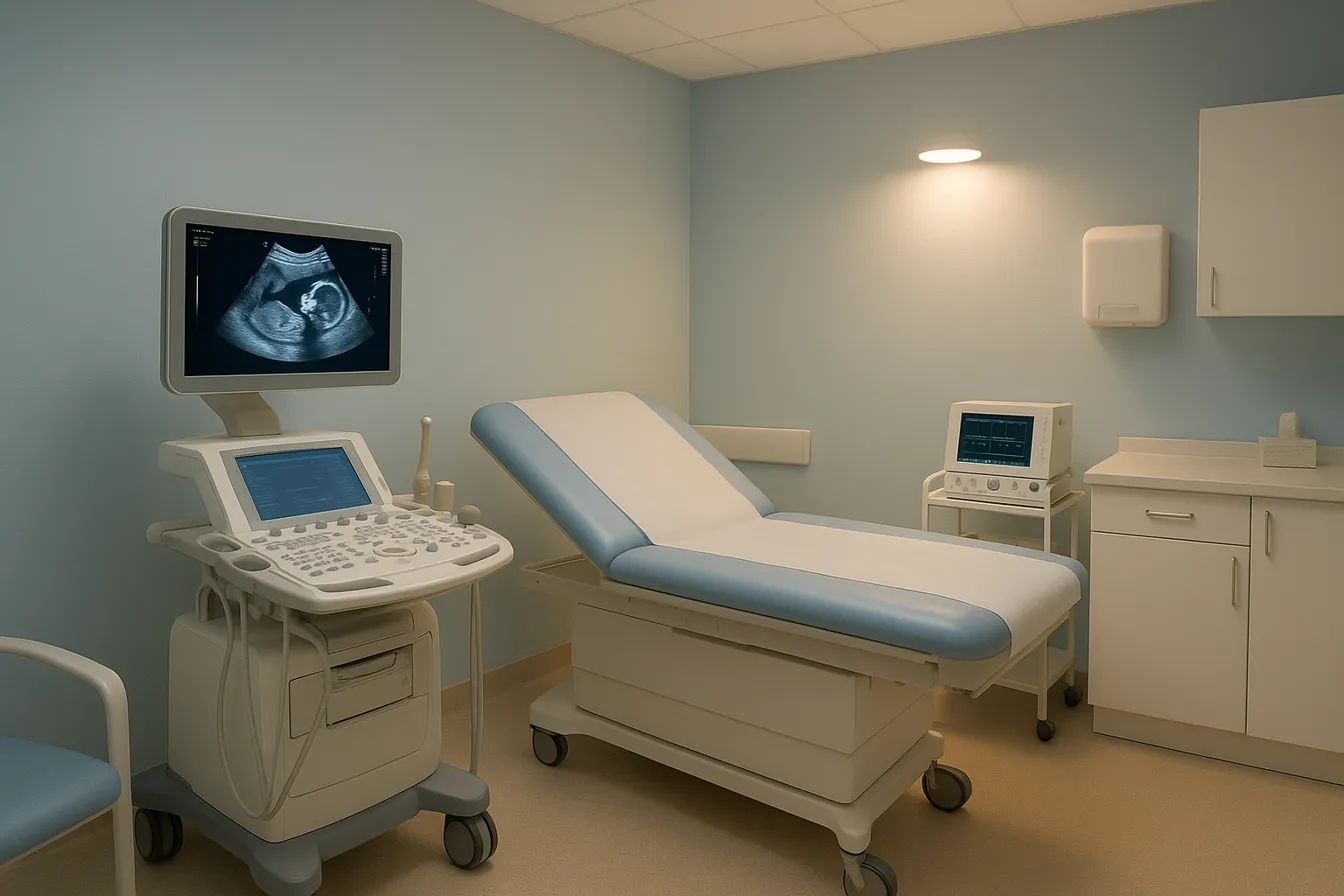
Pre-surgery Assessments and Tests
Before a myomectomy surgical procedure, thorough evaluation is essential to ensure safety and optimize outcomes. Patients typically undergo pelvic imaging such as ultrasound or MRI to assess fibroid size, number, and location. Blood tests including complete blood count are performed to check for anemia and prepare for possible transfusion. Additional assessments may include an electrocardiogram and chest X-ray to evaluate overall health.
Medication Management Including Blood Thinners
Managing medications is crucial before surgery to reduce bleeding risks. Patients are advised to stop blood-thinning drugs like aspirin, ibuprofen, naproxen, Clopidogrel, and warfarin several days prior, as directed by their healthcare provider. Iron supplements or hormone treatments such as GnRH agonists may be prescribed preoperatively to shrink fibroids and improve hemoglobin levels as part of preoperative preparations for myomectomy.
Fasting and Day-of Surgery Instructions
Patients must fast, typically avoiding food and drink after midnight before surgery to reduce anesthesia risks. On the day of surgery, only essential medications may be taken with a small sip of water. Arriving on time, following preoperative hygiene protocols such as showering without lotions or nail polish, and removing jewelry or piercings are important for safety and surgical readiness as outlined in preoperative instructions for fibroid removal.
Lifestyle Adjustments and Planning for Recovery
Lifestyle changes support a smoother recovery. Smoking cessation and avoiding alcohol at least 48 hours before surgery are strongly encouraged. Patients should arrange transportation, plan for rest and assistance at home, and prepare for activity restrictions after myomectomy. Nutrition and hydration pre- and postoperatively aid healing. Understanding and following surgeon instructions for postoperative care and activity limitations help prevent complications and support healing.
This comprehensive preparation ensures the patient is physically and mentally ready for surgery, improving safety and enhancing recovery.
Surgical Approaches: Types of Myomectomy Procedures and Their Benefits
What are the different types of myomectomy procedures?
Myomectomy procedures primarily include three surgical approaches: open abdominal myomectomy, laparoscopic and robotic-assisted myomectomy, and hysteroscopic myomectomy.
Open abdominal myomectomy: This involves a larger incision in the lower abdomen to remove fibroids. It is typically chosen for large fibroids or when multiple fibroids are present. Recovery can take four to six weeks.
Laparoscopic and robotic-assisted myomectomy: These minimally invasive gynecological surgery techniques use small incisions and cameras or robotic tools to remove fibroids. They are preferred for smaller or fewer fibroids. Recovery usually takes about two to four weeks.
Hysteroscopic myomectomy: This is the least invasive, involving the removal of fibroids through the vagina and cervix using a camera system, with no external incisions. It is suitable for submucosal fibroids under 4 cm and offers quick recovery in days.
How are procedures selected based on fibroid characteristics?
The choice depends on fibroid size, number, and location:
- Size: Large or numerous fibroids often require open abdominal myomectomy.
- Number: Multiple fibroids may necessitate open surgery.
- Location: Submucosal fibroids are usually treated with hysteroscopic myomectomy; intramural or subserosal fibroids may be managed via laparoscopic, robotic, or open methods.
What are the advantages and typical recovery times for each approach?
| Procedure Type | Advantages | Typical Recovery Time |
|---|---|---|
| Open abdominal myomectomy | Handles large/multiple fibroids; allows direct visualization | 4 to 6 weeks |
| Laparoscopic/robotic | Minimally invasive; less pain; smaller scars | 2 to 4 weeks |
| Hysteroscopic | No external incision; fast recovery; outpatient procedure | A few days to 2 weeks |
Each approach aims to relieve symptoms, preserve the uterus, and maintain fertility potential. Selection is tailored to the patient's fibroid characteristics and overall health.
What to Expect During the Myomectomy Procedure
Duration and Anesthesia
Myomectomy surgery generally lasts between two to three hours, depending on the size, number, and location of fibroids. It is performed under general anesthesia to ensure patient comfort and safety throughout the procedure.
Surgical Process Overview
The surgical approach is selected based on fibroid characteristics and patient goals. Open abdominal myomectomy involves a larger incision in the lower abdomen to remove fibroids, typically used for large or multiple growths. Minimally invasive myomectomy options include laparoscopic and robotic-assisted techniques, where small incisions are made, and specialized instruments with camera guidance are used to excise the fibroids. Hysteroscopic myomectomy is the least invasive, performed through the vagina without external incisions, suitable only for specific fibroids inside the uterine cavity.
Intraoperative Risks and Safety Measures
Potential risks during surgery include bleeding, infection, damage to surrounding organs, blood clots, and rare allergic reactions to anesthesia. Surgeons take comprehensive safety measures such as careful mapping of fibroid locations, meticulous surgical technique to minimize blood loss, and close monitoring of vital signs throughout. Blood samples are often taken before surgery to prepare for transfusion if necessary (preoperative instructions for fibroid removal).
Role of Advanced Techniques Such as Robotic Surgery
Robotic-assisted myomectomy utilizes the da Vinci® surgical system to enhance precision, maneuverability, and visualization. This advanced technology allows for more precise removal of fibroids with minimal trauma to surrounding tissues and typically results in shorter recovery times and smaller scars. It is especially beneficial for women desiring fertility preservation and seeking less invasive options compared to traditional open surgery.
Postoperative Recovery and Care After Myomectomy
Typical recovery timeline based on surgical approach
Recovery after myomectomy surgical procedure depends largely on the surgical method used. For open abdominal myomectomy, the healing period typically lasts 4 to 6 weeks. This approach involves a larger incision in the lower belly, requiring more time for tissue repair and overall recuperation. In contrast, minimally invasive myomectomy procedures such as laparoscopic or robotic-assisted myomectomy usually allow for recovery within 2 to 4 weeks, benefiting from small incisions and less surgical trauma. The least invasive is hysteroscopic myomectomy, performed through the vagina without external incisions, enabling patients to recover in just a few days.
Pain management and activity restrictions
Postoperative pain is common but can be effectively managed with prescribed medications and over-the-counter options like acetaminophen, ibuprofen, or naproxen as advised by your healthcare provider. Patients are encouraged to walk gently each day to improve circulation and prevent complications like blood clots. Heavy lifting, strenuous exercise, and other physically demanding activities should be avoided for 4 to 6 weeks after open surgery and for shorter periods after less invasive procedures. Sexual activity is generally restricted for about six weeks or until cleared by the doctor to allow complete healing. For more on pain management after myomectomy and activity restrictions after myomectomy, refer to official guidelines.
Incision care and wound management
For abdominal myomectomy, incision care after myomectomy is crucial. The surgical site should be kept clean and dry, with regular gentle washing using mild soap and water. Patients should avoid baths until their healthcare provider permits, usually after the first week. Tape strips or dressings left on by the surgeon should remain until advised for removal. Observing any signs of infection, such as redness, swelling, or discharge, is important for early intervention.
Postoperative symptoms and when to seek medical attention
Light vaginal bleeding or discharge is normal in the weeks following surgery. However, patients should seek immediate medical attention if they experience signs of excessive bleeding, severe abdominal pain unrelieved by medication, fever, signs of infection around the incision, or symptoms suggestive of blood clots such as leg swelling, chest pain, or shortness of breath. For detailed when to seek emergency care, consult your healthcare provider.
Tips to support healing and prevent complications
Adequate rest combined with gentle daily walking supports optimal healing and helps prevent issues like pneumonia and constipation. Staying hydrated and maintaining a balanced diet rich in fiber can also aid recovery. Avoiding smoking and following all post-surgical instructions from the healthcare team are essential for reducing risks of complications. Attend all follow-up care after myomectomy appointments to monitor healing progress and discuss any concerns with your medical provider.
Long-Term Outcomes and Fertility Considerations Post-Myomectomy
Impact on fertility and pregnancy outcomes
Myomectomy is often chosen by women who wish to preserve or improve fertility. Removing fibroids, especially those distorting the uterine cavity, can enhance the likelihood of conception and reduce miscarriage risks. However, not all fibroids equally affect fertility, and surgery mainly benefits those with submucosal types.
Risk of fibroid recurrence
Fibroids may recur after myomectomy, particularly in younger women and those with multiple fibroids initially. While the procedure alleviates symptoms and improves reproductive potential, ongoing monitoring is essential as new fibroids can develop, potentially necessitating further treatment.
Potential complications during pregnancy
A key consideration post-myomectomy surgical procedure is the risk of uterine rupture during pregnancy due to surgical incisions in the uterine wall. This risk varies with the surgical approach and extent of uterine repair. Consequently, cesarean delivery is frequently recommended to ensure safety. Other pregnancy-related complications might include a higher probability of cesarean section and the need for specialized prenatal care.
Menstrual cycle changes after surgery
Most women experience lighter and more regular menstrual periods following myomectomy surgical procedure. Symptom relief from heavy bleeding and pelvic pain is common, contributing to improved quality of life.
Follow-up care and monitoring
Postoperative care includes regular follow-up visits to assess healing, manage any complications, and monitor for fibroid recurrence. Patients are advised to wait three to six months before attempting pregnancy to allow uterine healing. Screening and tailored advice help optimize reproductive outcomes and overall health.
The Role of Woman-Led Healthcare Providers in Women’s Health and Fibroid Care
What are the comprehensive obstetrics and gynecology services offered by a woman-led healthcare provider?
A woman-led healthcare provider specializing in obstetrics and gynecology offers a full spectrum of care tailored to women's unique health needs. Services include routine gynecological exams like Pap smears and mammograms, management of reproductive health issues such as polycystic ovary syndrome and endometriosis, and specialized prenatal care throughout pregnancy. They also provide labor and delivery support, postpartum follow-up, family planning, contraception counseling, and hormonal therapies. These providers create a welcoming environment that supports women's mental, emotional, and physical well-being.
How does personalized and advanced women's health care benefit patients?
Personalized healthcare customizes treatments to fit individual medical histories, lifestyles, and specific health concerns, resulting in more effective management and better outcomes. Incorporating advanced diagnostic tools allows earlier detection of conditions, enabling proactive care. Women receiving this focused care often report greater satisfaction and a stronger patient-provider bond, encouraging active engagement in their health decisions and care plans.
What distinguishes a woman-led healthcare provider in the field of women's health?
Woman-led healthcare providers bring an empathetic and deeply informed perspective grounded in both professional expertise and lived experience. Their leadership fosters a patient-centered approach that prioritizes women's unique health concerns and encourages empowerment and shared decision-making. These providers often advocate for progress in women's health research and equitable access to care, shaping a supportive environment specifically designed for female patients.
What are the latest advancements in obstetrics and gynecology that improve patient care?
Advancements include minimally invasive surgeries like laparoscopic myomectomy and robotic-assisted procedures that shorten recovery and reduce complications. Enhanced prenatal screening with advanced ultrasound and genetic testing improves early detection of potential issues. Telehealth has expanded access to care, particularly for women in remote locations. Personalized hormone therapies and innovative fertility treatments offer tailored, effective options that address individual patient needs across different life stages.
Final Thoughts on Fibroid Myomectomy and Patient Empowerment
Understanding Fibroid Myomectomy
Myomectomy is a surgical procedure aimed at removing uterine fibroids while preserving the uterus, crucial for women wishing to maintain fertility. Different surgical techniques—including abdominal, laparoscopic, robotic-assisted, and hysteroscopic—offer tailored options based on fibroid size, location, and number. Recovery times vary, with minimally invasive approaches allowing faster return to normal activities.
Personalized Care and Informed Decisions
Choosing the right myomectomy approach depends on each patient’s individual condition and reproductive goals. Preoperative planning, clear communication about risks and benefits, and thorough follow-up care are essential for optimal outcomes. Patients should feel empowered to ask questions and weigh treatment options carefully.
Support from Woman-Led Providers
Women benefit from consulting healthcare providers who specialize in women's health and understand their unique needs. Woman-led teams often provide compassionate, patient-centered care that supports both physical and emotional well-being throughout diagnosis, treatment, and recovery.
Empowerment through knowledge and personalized care is the foundation for successfully managing fibroids and preserving fertility.



.png)