Comprehensive Preventive Care for Women: Tailoring Screenings and Wellness Across the Lifespan

Introduction to Minimally Invasive OB/GYN Surgeries and Their Benefits
Overview of Laparoscopic OB/GYN Surgery
Laparoscopic surgery in obstetrics and gynecology is a minimally invasive technique that employs small incisions to insert a laparoscope—a slender device equipped with a camera—into the abdomen. This approach allows surgeons to view pelvic organs and perform precise procedures with less trauma to healthy tissue.
Less Invasive Approach Compared to Traditional Surgery
Unlike open surgery that requires large incisions, laparoscopy leaves just a few small scars, typically less than a centimeter in size. Patients experience significantly less tissue disruption, which reduces blood loss and lowers the risk of infection.
General Benefits Including Faster Recovery and Fewer Complications
The minimally invasive nature of laparoscopic OB/GYN surgeries offers major advantages. Patients often enjoy less postoperative pain and shoulder discomfort from residual gas. Because most procedures are outpatient, recovery is quicker, allowing a return to normal activities within days to weeks. Smaller scars and fewer complications such as infections or blood clots contribute to an overall safer and more comfortable healing process.
What Is Laparoscopic Surgery and How Does It Benefit Women?

Definition and Technical Aspects of Laparoscopy
Laparoscopic surgery, often called minimally invasive surgery, is a technique that uses small incisions in laparoscopy, approximately the size of a buttonhole, to perform surgical procedures. A laparoscope device with camera—a slender, lighted tube with a tiny camera—is inserted through one of these incisions, usually near the belly button. This camera transmits high-definition images to a monitor, allowing the surgeon to view and operate on pelvic and abdominal organ visualization precisely.
Common Gynecological Conditions Treated
This surgical method is widely used to diagnose and treat various gynecological conditions, including endometriosis treatment, ovarian cyst surgery laparoscopy, fibroids treatment with laparoscopy, ectopic pregnancy laparoscopy, pelvic pain, infertility issues, and pelvic floor disorders. It also assists in procedures like hysterectomy, tubal ligation, and removal of scar tissue, offering versatile treatment options for women.
Comparison with Open Surgery: Incisions and Healing
Compared to traditional open surgery, laparoscopy involves far smaller incisions surgery, leading to significantly less tissue trauma. This minimally invasive laparoscopy approach reduces blood loss, lowers the risk of infection, and decreases postoperative swelling. Smaller incisions mean fewer stitches and generally quicker wound healing. The procedure often allows for outpatient laparoscopic procedures, enabling many patients to return home within hours and resume normal activities more rapidly.
Smaller Scars and Less Postoperative Pain
The small size of the incisions results in less scarring with laparoscopy over time. Additionally, because laparoscopy causes less disruption to surrounding tissues, patients typically experience lower pain after laparoscopy and discomfort. This reduced pain allows for early mobilization, promoting faster recovery with laparoscopy and a better overall healing experience. Shoulder pain caused by residual gas used during the operation may occur but usually resolves shortly after surgery.
Overall, laparoscopic surgery represents a major advancement in women's healthcare, providing effective treatment with enhanced safety, quicker recovery, and improved cosmetic outcomes compared to traditional methods.
Key Advantages of Laparoscopic OB/GYN Surgery for Faster Recovery
Reduced postoperative pain and trauma
Laparoscopic surgery uses tiny incisions and precise instruments, which reduce damage to surrounding tissues. This minimally invasive laparoscopy approach leads to significantly less postoperative pain compared to traditional open surgery. Patients often experience less discomfort in their abdomen and shoulders, allowing for easier managing laparoscopy pain and overall improved comfort during recovery.
Smaller incisions and minimal scarring
The incisions made during laparoscopic procedures are generally about the size of a buttonhole (0.5 to 1.5 cm). These small incisions in laparoscopy require fewer stitches and heal with barely noticeable scars. This cosmetic benefit also lowers the risk of adhesion formation and scar tissue, contributing to better long-term outcomes.
Lower risk of infection and blood loss
Because laparoscopy involves smaller cuts and less tissue trauma, it reduces the likelihood of surgical site infections and hemorrhage. The enhanced visualization with the laparoscope allows surgeons to operate with greater precision, further minimizing blood loss and complications.
Outpatient procedures and quicker hospital discharge
Many outpatient laparoscopic procedures OB/GYN surgeries are performed on an outpatient basis, meaning most patients go home the same day or within 24 hours. This shorter hospital stay decreases exposure to hospital-related risks, lowers healthcare costs, and supports faster emotional and physical recovery.
Faster return to daily activities
Recovery times for laparoscopic surgeries are significantly shorter. Many patients resume normal activities such as walking, driving, and light work within a few days. More minor procedures allow return to work within one to two weeks, while more complex surgeries might require several weeks but still remain quicker than open surgery outcomes.
Advantages of specialized OB/GYN care
Healthcare providers specialized exclusively in obstetrics and gynecology bring focused expertise to women's health. They manage complex reproductive and hormonal conditions, perform cancer screenings, and address mental and pelvic health concerns. Their focused training ensures personalized care and trust-building, optimizing health outcomes throughout a woman's life.
| Benefit | Description | Patient Impact |
|---|---|---|
| Less pain & trauma | Small incisions & precise tools reduce tissue damage | Improved comfort & pain control |
| Minimal scarring | Buttonhole-size cuts lead to less visible scars | Better cosmetic results |
| Lower infection & blood loss | Reduced trauma lowers complications | Safer surgeries & faster healing |
| Outpatient procedures | Most surgeries done same day or short hospital stays | Less exposure, faster emotional & physical recovery |
| Quicker activity return | Rapid healing supports early resumption of daily tasks | Faster independence & quality of life |
| Specialized OB/GYN expertise | Focused women's health care and personalized treatment | Holistic health & trust in care |
Enhanced Recovery After Surgery (ERAS) and Its Role in Laparoscopic Gynecologic Procedures

What are ERAS pathways and how do they optimize perioperative care?
Enhanced Recovery After Surgery (ERAS pathways) are comprehensive, evidence-based protocols designed to maintain normal body functions and improve recovery quality throughout the perioperative period. For laparoscopic gynecologic surgeries, ERAS emphasizes preoperative education, nutritional optimization, and tailored anesthesia techniques. This approach reduces stress on the body during surgery, minimizes complications, and prepares patients physically and mentally to recover swiftly.
How is pain managed and mobilization encouraged after laparoscopic surgery?
Pain management within ERAS uses a multimodal strategy combining non-opioid analgesics like NSAIDs and acetaminophen, regional anesthesia, and minimal opioid use to keep discomfort low without side effects. Early mobilization, including sitting and walking usually from the day of surgery, is actively encouraged. This helps ease pelvic muscle spasms, enhances bowel function, and reduces risks such as blood clots (Tips for recovering from laparoscopy).
What benefits does ERAS offer in hospital stay length and bowel recovery?
Following ERAS protocols results in shorter hospital stays or outpatient care for many laparoscopic procedures. Early feeding and mobilization accelerate bowel function recovery, reducing postoperative nausea and constipation. These factors enable most patients to return to their normal activity levels quicker than with traditional perioperative care (Enhanced Recovery After Surgery pathways.
How does multidisciplinary care and patient education contribute to ERAS success?
Successful ERAS depends on collaboration among surgeons, anesthesiologists, nurses, and physical therapists. Clear patient education about pre-surgery preparation, pain control, activity resumption, and wound care empowers women to actively participate in their recovery. This personalized approach improves adherence to protocols and addresses individual needs effectively (Enhanced Recovery After Surgery benefits).
What is the impact of ERAS on patient satisfaction and complication rates?
Implementation of ERAS pathways in laparoscopic gynecologic surgery reduces postoperative pain and complication rates, such as infections and thromboembolism. Patients report higher satisfaction due to better pain control, faster recovery, and shorter hospital stays. Studies confirm ERAS does not increase readmissions or reoperation rates, making it a safe and patient-centered standard for gynecologic laparoscopy (Enhanced Recovery After Surgery (ERAS) protocols.
How does personalized care improve outcomes in women's health services?
Personalized care greatly enhances women's health by considering unique hormonal, reproductive, and genetic factors influencing health and treatment. Tailoring therapies and preventive strategies—supported by technology like telemedicine and AI—allows for more precise diagnosis and targeted interventions. This individualized approach promotes better prevention, chronic condition management, and increased patient engagement, resulting in improved overall outcomes.
| ERAS Component | Description | Benefit |
|---|---|---|
| Preoperative Optimization | Education, nutrition, smoking cessation | Faster, safer surgery (ERAS in gynecologic surgeries |
| Multimodal Pain Control | NSAIDs, acetaminophen, regional anesthesia | Less opioid use, better pain relief |
| Early Mobilization | Walking and breathing exercises soon after surgery | Reduced complications, faster bowel health (Tips for recovering from laparoscopy |
| Multidisciplinary Teamwork | Coordinated care among all providers | Enhanced recovery consistency |
| Patient Education | Informing patients on expectations and care | Greater adherence and satisfaction |
| Shorter Hospital Stay | Outpatient or minimal admission | Reduced costs, quicker home recovery (Outpatient laparoscopic procedures) |
Preoperative Preparation and Postoperative Care for Optimal Recovery
Why is preoperative health optimization important?
Maintaining good health before minimally invasive gynecologic surgery can significantly improve recovery outcomes. Patients are encouraged to adopt a healthy diet, quit smoking at least three weeks prior, and reduce stress to aid healing. Timing surgery just after menstruation may reduce uterine cramps and facilitate a smoother procedure. For more on preparing for laparoscopy surgery, visit the linked resource.
How are pain management and muscle spasm control addressed after surgery?
Minimally invasive laparoscopy typically results in less postoperative pain. However, pelvic muscle spasms may cause discomfort that surgery alone cannot treat. Effective pain control includes prescribed painkillers and strategies to minimize opioid use after 2–3 days. Managing muscle spasms with gentle pelvic stretches and minimizing constipation also helps reduce pain as noted in Tips for recovering from laparoscopy.
What are the recommendations for early mobilization and activity?
Patients are encouraged to begin light activities such as short walks the day after surgery to promote bowel function and reduce muscle spasms. Gradual resumption of daily tasks supports faster recovery. Driving and sexual activity should be resumed only after clearance by healthcare providers. Contact sports and heavy lifting should be avoided until fully healed. Refer to Laparoscopy activity guidelines for detailed recommendations.
How can common postoperative symptoms be managed?
Shoulder pain from residual carbon dioxide gas used during surgery, vaginal bleeding for 24–48 hours, fatigue, and abdominal soreness are common but typically temporary. Staying hydrated, maintaining a balanced diet, and resting adequately promote symptom resolution. Monitoring for complications like fever, increased pain, or wound redness is essential as explained in Postoperative symptoms after laparoscopy.
What role does patient education and support play in recovery?
Comprehensive preoperative counseling about the surgical process, expected symptoms, and recovery timelines enhances patient confidence and compliance. Understanding the benefits of early mobilization, pain control, and wound care empowers patients to take active roles in their recovery. Access to multidisciplinary support services further improves outcomes and satisfaction. Insights on gynecological surgeon tips can be helpful.
Technological Advances and Surgical Innovation in Minimally Invasive Gynecologic Surgery

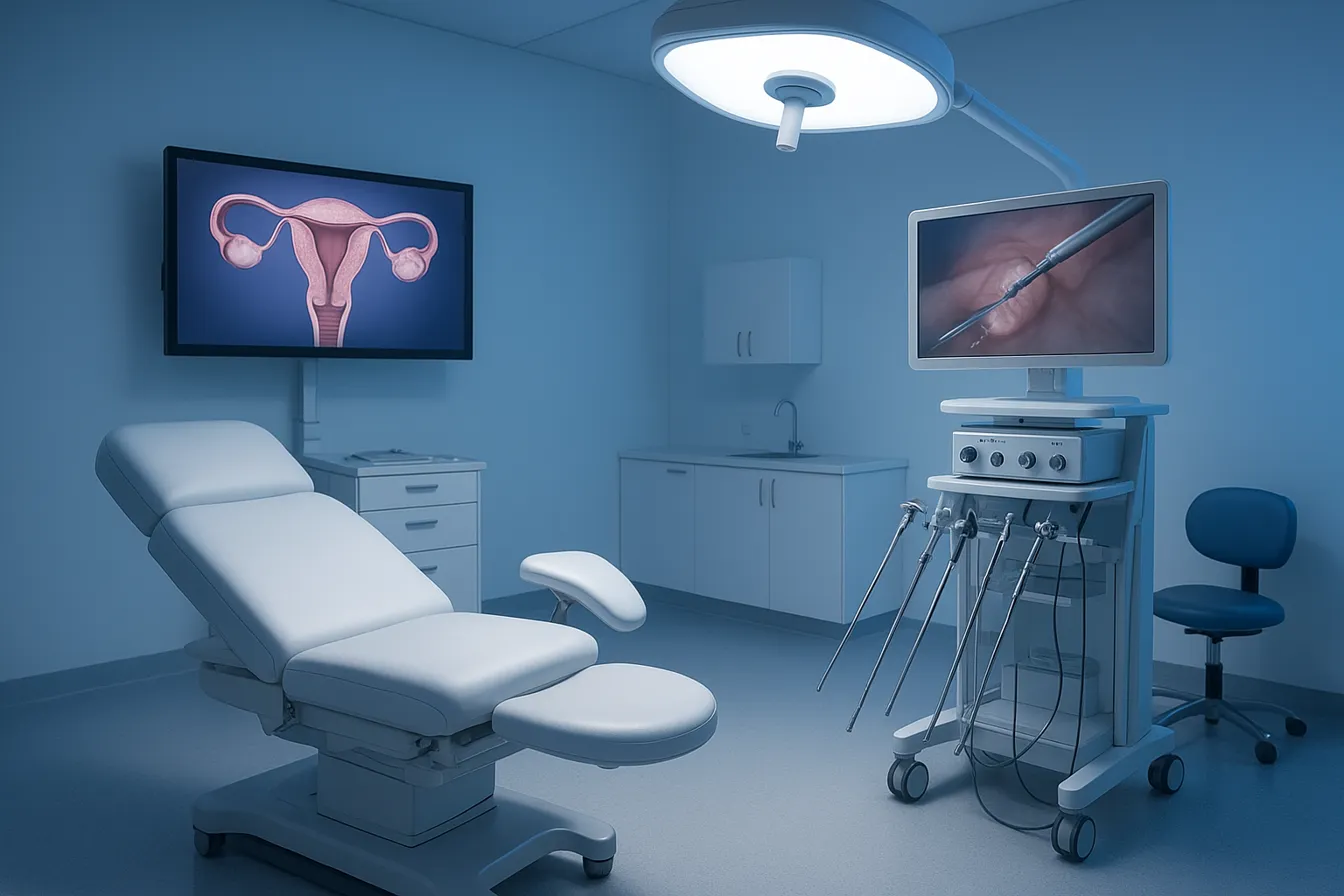
Use of High-Definition Imaging and Precision Instruments
Minimally invasive gynecologic surgery leverages high-definition imaging provided by laparoscopes — long, slender devices equipped with cameras and light sources. This technology offers surgeons a magnified, clear view of pelvic and abdominal organs, enabling precise surgical maneuvers through very small incisions in laparoscopy. Specialized thin surgical tools complement this visualization, allowing minimal tissue trauma and reducing blood loss and infection risks.
Robotic-Assisted Laparoscopy and Advanced Laparoscopy Techniques
Robotic-assisted laparoscopy enhances precision by providing 3D magnified views and fine instrument control. This advancement facilitates complex procedures such as laparoscopic hysterectomy and myomectomy with improved accuracy and reduced postoperative discomfort. Surgeons trained in advanced laparoscopic methods utilize barbed sutures and improved entry techniques like Veress needle or open Hasson approaches, optimizing operative efficiency and safety (minimally invasive gynecological surgery benefits).
Emerging Procedures: vNOTES and Radiofrequency Ablation
Innovations such as vaginal natural orifice transluminal endoscopic surgery (vNOTES) and transcervical radio-frequency ablation (e.g., the Sonata system) represent next-generation options. vaginal natural orifice transluminal endoscopic surgery (vNOTES) eliminates abdominal incisions by using vaginal access, resulting in no visible scarring and faster recovery. Radiofrequency ablation treats fibroids internally without skin incisions, minimizing tissue damage and promoting quicker healing.
Benefits of Smaller or No Incisions and Improved Surgical Accuracy
Smaller incisions — often less than a centimeter — or no abdominal incisions translate to less postoperative pain, minimal scarring, and quicker return to daily activities. Enhanced visualization and surgical precision reduce complication rates, blood loss, and hospital stays. Patients frequently experience outpatient laparoscopic procedures with rapid recovery timelines.
Training and Quality Standards in Women-Led Healthcare Practices
Excellence in minimally invasive gynecologic surgery depends on specialized surgeon training, often including fellowship certifications and simulation-based surgical training in laparoscopy. Women-led healthcare centers prioritize multidisciplinary collaboration and evidence-based protocols to maintain high care quality. Centers of Excellence, such as UConn Health Center of Excellence for Minimally Invasive Gynecologic Surgery, showcase these rigorous standards fostering safe, innovative, and patient-centered surgical approaches.
Patient Experience and Long-Term Benefits of Laparoscopic OB/GYN Surgeries
How Does Faster Recovery Improve Quality of Life?
Laparoscopic OB/GYN surgeries use Small incisions in laparoscopy, resulting in Less post-operative pain after laparoscopic surgery and quicker healing. Patients typically return to normal activities within days to weeks, compared to longer recovery times for open surgery. This swift recovery reduces time away from work and daily routines, supporting a faster return to family and social life.
What Are the Reduced Risks of Complications and Readmissions?
Minimally invasive laparoscopic surgery minimize trauma to tissues and blood loss, lowering infection risks. Studies show fewer complications such as wound infections and blood clots, which translate to decreased hospital stays and reduced readmissions. Enhanced Recovery After Surgery (ERAS) pathways further improve outcomes by standardizing care and promoting early mobilization and nutrition.
What Are the Psychological Benefits of Less Pain and Scarring?
Smaller incisions mean Less scarring with laparoscopy and discomfort. Patients often experience less anxiety about surgery and body image concerns. Less pain after laparoscopy also leads to lower reliance on opioids, which decreases the risk of prolonged pain sensitivity and supports emotional well-being during recovery.
How Do Supportive and Personalized Care Environments Contribute?
Comprehensive perioperative education and tailored pain management help patients manage expectations and recovery effectively. Collaborative care involving multidisciplinary teams ensures advanced surgical techniques are combined with patient-specific strategies, fostering confidence and satisfaction.
What Is the Overall Impact on Women’s Health and Wellbeing?
Laparoscopic surgery advances not only improve physical healing but also enhance overall quality of life by minimizing disruption and promoting faster functional restoration. These benefits extend to managing conditions like endometriosis, fibroids, and pelvic pain, enabling sustained health improvements and improved daily functioning for women.
| Aspect | Benefit | Explanation |
|---|---|---|
| Recovery Time | Faster recovery laparoscopy | Small incisions in laparoscopy |
| Complication Risks | Lower complication risk with laparoscopy | Less tissue trauma lowers infection and blood loss |
| Psychological Impact | Benefits of laparoscopy | Postoperative pain reduction laparoscopic surgery |
| Patient Care | Enhanced Recovery After Surgery (ERAS) pathways | Laparoscopic gynecological surgery |
| Long-Term Wellbeing | Benefits of laparoscopic gynecrological procedures | Benefits of laparoscopy |
Conclusion: Laparoscopic OB/GYN Surgeries as a Pathway to Superior Recovery and Care
Benefits of Laparoscopic Surgery
Laparoscopic OB/GYN surgeries offer numerous advantages including smaller incisions, reduced pain, faster recovery, fewer complications, minimal scarring, and shorter hospital stays. This minimally invasive approach allows women to return to daily activities more quickly and with less discomfort than traditional surgery.
Specialized, Women-Centered Care
These procedures are often performed by highly trained specialists focused on women's health, ensuring personalized and compassionate treatment. The use of advanced technology and expertise improves surgical precision and patient outcomes.
Embracing Minimally Invasive Options
Patients and providers are encouraged to consider laparoscopic techniques when possible, as they represent a state-of-the-art approach that supports faster healing, fewer risks, and a better overall experience. This commitment to minimally invasive care is pivotal for enhancing women's health and quality of life.



.png)