Navigating Women's Health: A Comprehensive Guide Across Life Stages

Introduction to Uterine Fibroids and Their Impact
What Are Uterine Fibroids?
Uterine fibroids, also known as leiomyomas, are common noncancerous tumors that develop in the muscular wall of the uterus. They affect a large number of women, with statistics showing that up to 80% of women may have fibroids by the age of 50. These growths vary widely in size — from as small as a seed to larger than a watermelon — and are influenced by hormones, mainly estrogen and progesterone.
Symptoms and Effects on Health
While many women with fibroids have no symptoms, others experience significant issues such as heavy or prolonged menstrual bleeding, pelvic pain, pressure or fullness, frequent urination, and complications affecting fertility and pregnancy. Symptoms can greatly impact quality of life, sometimes leading to anemia or difficulty conceiving.
The Need for Individualized Care
Because fibroids differ in number, size, and location as well as in symptom severity and patient reproductive goals, treatment requires a tailored approach. Some women may benefit from watchful waiting, while others need a range of options from medication to minimally invasive procedures or surgery. Personalized care ensures that treatment aligns with the specific needs and preferences of each patient, improving outcomes and well-being.
Diagnosis of Uterine Fibroids: Tools and Techniques
Role of pelvic exams in detecting fibroids
Uterine fibroids are often discovered during routine pelvic exams, where a healthcare provider may notice irregularities in the shape or size of the uterus. These physical findings, such as a uterine enlargement or asymmetry, can suggest the presence of fibroids even in women without noticeable symptoms. Pelvic exams serve as an important first step in identifying women who may need further diagnostic testing.
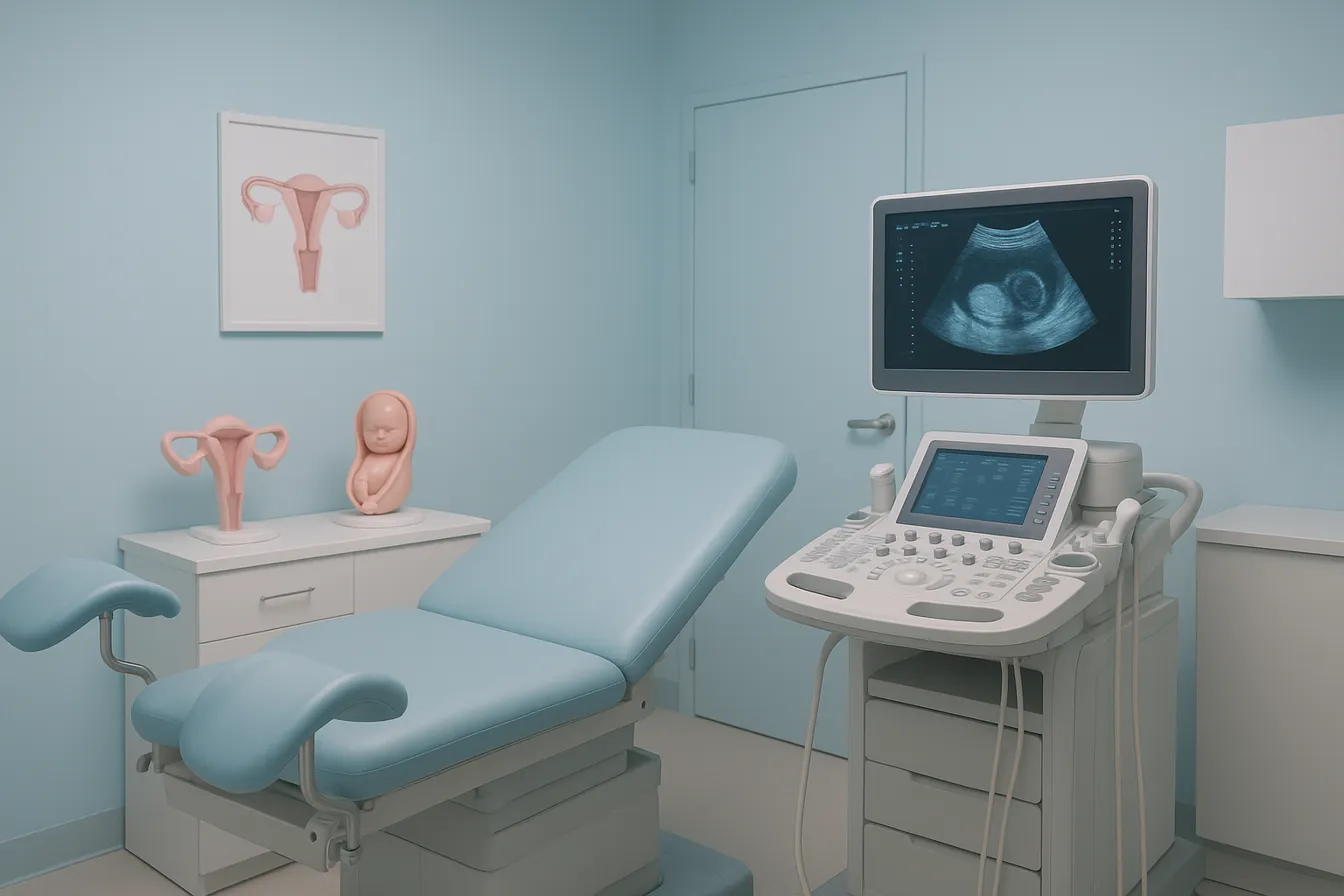
Ultrasound modalities including transvaginal and transabdominal as primary diagnostics
Ultrasound is the cornerstone of uterine fibroids diagnosis. Both transvaginal ultrasound and transabdominal ultrasound methods are routinely utilized to confirm the presence of fibroids, determine their number, exact location, and measure their size. Transvaginal ultrasound provides higher-resolution images, especially useful for evaluating fibroids located inside or near the uterine cavity, while transabdominal ultrasound offers a broader view of the pelvis. This noninvasive and readily accessible technology plays a critical role in initial assessment and ongoing monitoring of fibroids.
Use of advanced imaging like MRI, hysterosonography, and hysteroscopy for detailed assessment
When ultrasound findings are inconclusive or more detailed visualization is required, advanced imaging and diagnostic techniques may be employed. Magnetic resonance imaging (MRI) offers detailed visualization of fibroid size and location, especially in larger uteri or when fibroids are numerous. Hysterosonography, which involves saline infusion during ultrasound, enhances the view of the uterine lining and is particularly valuable for identifying submucosal fibroids affecting fertility or causing heavy bleeding. Hysteroscopy allows direct endoscopic inspection of the uterine cavity and can also aid in biopsy or minimally invasive treatment. These specialized techniques facilitate a comprehensive understanding of fibroid impact on uterine anatomy.
Importance of individualized diagnostic approach based on symptoms and fertility goals
Diagnostic evaluations for uterine fibroids are tailored to each woman's symptoms, clinical context, and reproductive plans. For asymptomatic women or those with mild symptoms, a less invasive approach with routine imaging may suffice. In contrast, women experiencing heavy bleeding, pain, or infertility often require more detailed assessment through hysterosonography or MRI to guide treatment strategies effectively. Collaboration between the patient and healthcare provider ensures an optimal, personalized diagnostic and management plan that respects fertility desires while addressing symptom severity.
Symptomatology of Fibroids: When Treatment Becomes Necessary
Common symptoms including heavy menstrual bleeding, pelvic pressure, pain, and fertility issues
Uterine fibroids overview frequently cause symptoms such as heavy or prolonged menstrual bleeding, which may lead to anemia if untreated. Pelvic pressure or fullness is common, often accompanied by pain during menstruation or intercourse, as well as lower back pain and urinary frequency. Fibroids can also affect fertility and pregnancy outcomes, particularly when located in the submucosal region of the uterus, potentially increasing miscarriage risk and complicating labor.
Prevalence of asymptomatic fibroids and rationale for watchful waiting
Despite their high prevalence—up to 80% of women by age 50—a significant proportion of women with fibroids remain asymptomatic. For these patients, watchful waiting is the preferred approach as many fibroids grow slowly or shrink after menopause. As fibroids are benign and noncancerous in most cases, immediate treatment is not necessary unless symptoms worsen or impact quality of life.
Impact of fibroids on quality of life and reproductive outcomes
Symptomatic fibroids can markedly reduce quality of life through heavy bleeding leading to fatigue, pain, and pelvic discomfort. For women of reproductive age, fibroids may reduce fertility and increase the risk of pregnancy complications, including cesarean delivery, preterm birth, and fetal growth restriction.
Risks of complications such as anemia and pregnancy challenges
Heavy menstrual bleeding from fibroids can cause significant anemia, requiring medical intervention. During pregnancy, fibroids may grow due to elevated hormone levels and contribute to complications like miscarriage, preterm rupture of membranes, and labor difficulties. Close monitoring and individualized treatment plans are essential to manage these risks effectively.
Medical Management of Fibroids: Hormonal and Non-Hormonal Approaches

Medications for Symptom Relief
Management of uterine fibroids symptoms often starts with medications aimed at controlling bleeding and pain. NSAIDs for fibroid pain are commonly used to reduce pain by decreasing prostaglandin production, which alleviates heavy menstrual bleeding and discomfort. Tranexamic acid for bleeding, an antifibrinolytic agent, is effective during heavy menstrual bleeding days by helping reduce blood loss by approximately 40-50%. Hormonal contraceptives, including combined oral contraceptives and progestins, are also prescribed to manage abnormal uterine bleeding, with contraceptives additionally providing contraceptive benefits. These medications typically do not shrink fibroids but improve quality of life by controlling symptoms.
Gonadotropin-Releasing Hormone (GnRH) Agonists and Antagonists
GnRH agonists treatment such as leuprolide induce a temporary menopause-like state that substantially shrinks fibroids—by about 50% after three months of use—and reduce bleeding. However, their use is limited to short durations due to side effects including hot flashes and bone density loss. GnRH antagonists therapy, including elagolix and relugolix, offer an alternative with a potentially better safety profile for longer-term use. These medications reduce menstrual bleeding and may help control fibroid size but are generally considered a temporary measure or used prior to surgery.
Progestin-Releasing Intrauterine Devices (IUDs)
The Progestin-releasing IUD such as the levonorgestrel-releasing intrauterine system (LNG-IUS) is effective in treating heavy menstrual bleeding linked to fibroids by thinning the uterine lining. While this device can reduce bleeding significantly and improve symptoms, it does not reduce fibroid size. Expulsion risk is higher in women with fibroids larger than 3 cm, but LNG-IUS remains a valuable symptom management tool, especially for those seeking fertility preservation.
Emerging Therapies and Risk Profiles
Selective progesterone receptor modulators (SPRMs), such as ulipristal acetate, have shown initial promise in reducing bleeding and fibroid volume. However, due to risks of severe liver injury, their use is restricted and requires careful monitoring. Other hormonal modulators like mifepristone and letrozole are being studied for symptom control. The emergence of newer GnRH antagonists therapy with improved safety profiles offer hope for longer-term medical management. Despite these advances, no medication currently provides a permanent cure, and fibroids may recur or regrow when treatment is stopped.
Medical management strategies should be individualized, balancing benefits and risks while considering patient symptoms, fertility goals, and treatment preferences, with consultation from healthcare providers essential for effective care.
Minimally Invasive and Non-Surgical Treatments: Advancing Fibroid Care

What is uterine artery embolization (UAE) and how effective is it?
UAE is a minimally invasive procedure that blocks the blood supply to fibroids, causing them to shrink. It typically results in fibroid size reduction by about 30-50%, with most patients experiencing significant symptom relief. Performed by interventional radiologists, UAE involves catheter insertion through a small groin incision and usually allows patients to go home the same day. Recovery is faster than traditional surgery.
How does MRI-guided focused ultrasound surgery (FUS) work as a noninvasive treatment?
FUS uses MRI to guide high-energy ultrasound waves to destroy fibroid tissue without incisions. This outpatient procedure preserves the uterus and is suitable for women seeking noninvasive options. Patients may feel warmth or cramping during treatment. While it offers a shorter recovery period, the long-term effectiveness and safety continue to be studied.
What are the benefits of laparoscopic radiofrequency ablation and hysteroscopic myomectomy?
Laparoscopic radiofrequency ablation destroys fibroids using heat delivered through small abdominal incisions, resulting in less pain, fewer complications, and quicker recovery than open surgery. Hysteroscopic myomectomy removes fibroids confined within the uterine cavity via a thin scope through the vagina. Both approaches aim to relieve symptoms with minimal invasion.
How do these treatments consider fertility preservation in fibroid treatment and risk of fibroid recurrence after treatment?
Myomectomy procedures, including laparoscopic and hysteroscopic methods, are preferred for women desiring future pregnancies as they preserve the uterus. UAE and FUS typically spare the uterus but their impacts on fertility are less certain. Fibroids may recur or new ones develop after conservative treatments, warranting ongoing monitoring and personalized care decisions.
Surgical Interventions: Myomectomy and Hysterectomy
When Is Surgery Recommended for Fibroids?
Surgical treatment of uterine fibroids is typically considered when fibroids cause significant symptoms such as heavy menstrual bleeding, pelvic pain, or pressure symptoms affecting bladder or bowel function. Surgery may also be recommended based on the size and location of fibroids, especially if they distort the uterine cavity or impact fertility. Women who wish to preserve fertility often lean towards surgery to remove fibroids causing reproductive difficulties.
Myomectomy: Techniques and Fertility Preservation
Myomectomy is the surgical removal of fibroids while preserving the uterus, making it the preferred option for women who want to maintain fertility. Several techniques are used depending on fibroid size, number, and location:
- Open (Abdominal) Myomectomy: Involves a larger incision, generally reserved for multiple or very large fibroids.
- Laparoscopic Myomectomy: A minimally invasive approach using small incisions and a camera, offering less blood loss and quicker recovery.
- Robotic-Assisted Myomectomy: A refined laparoscopic technique with enhanced precision using robotic instruments.
These procedures aim to remove fibroids effectively while preserving uterine integrity. However, myomectomy carries a risk of fibroid recurrence ranging from 15% to 33%, and requires skilled surgical expertise.
Hysterectomy: Definitive Treatment and Considerations
Hysterectomy—the complete removal of the uterus—is a definitive treatment for fibroids, providing complete symptom resolution. It is recommended when fibroids are very large, numerous, or when fertility preservation is not a concern. Recovery times vary by surgical approach, with vaginal hysterectomy offering shorter operative times and faster recovery compared to abdominal surgery. Since hysterectomy eliminates fertility, it is reserved for women who do not desire future pregnancies.
Morcellation Risks and Safety Recommendations
Morcellation is a technique used in minimally invasive myomectomy and hysterectomy to fragment large fibroids for removal through small incisions. However, it carries a risk of spreading undiagnosed uterine cancer (such as leiomyosarcoma) within the abdominal cavity. To mitigate these risks, the FDA advises caution or avoidance of power morcellators, especially in women nearing or after menopause. Use of contained or enclosed morcellation bags and thorough preoperative evaluation helps reduce cancer spread risk.
Women considering surgical options should have detailed discussions with their healthcare providers about fertility goals, risks, benefits, and recovery expectations to choose the most appropriate intervention.
Recurrence and Long-Term Outcomes After Fibroid Treatment
What Are the Rates of Fibroid Recurrence After Treatment?
Fibroid recurrence is a recognized issue following treatments that preserve the uterus, such as myomectomy. Studies indicate that recurrence rates after myomectomy range from 15% to 33%, with some patients eventually requiring additional interventions including hysterectomy. Minimally invasive treatments like uterine artery embolization (UAE) report reintervention rates between 20% and 33% over several years. These rates highlight that fibroid removal or shrinkage does not guarantee permanent resolution.
Is It Possible for New Fibroids to Develop After Treatment?
Yes, new fibroids can develop even after treatment, reflecting the multifocal nature of this condition. Procedures that do not remove the uterus entirely, including myomectomy and UAE, leave the uterine environment that can support new fibroid growth. This potential for new fibroids requires ongoing monitoring, especially in women wishing to preserve fertility (impact of fibroids on fertility outcomes).
How Do Surgical and Minimally Invasive Procedures Compare Long-Term?
Traditional surgical treatments like hysterectomy provide definitive fibroid resolution but sacrifice fertility. Myomectomy preserves the uterus but carries a recurrence risk. Minimally invasive options such as uterine artery embolization and MRI-guided focused ultrasound offer uterus preservation with shorter recovery times and fewer complications. However, these techniques have higher rates of fibroid recurrence and symptom return compared to hysterectomy. Patient preferences, symptom severity, and reproductive plans guide the choice of intervention.
Why Is Individualized Follow-Up Important?
Given the variable recurrence rates and the possibility of symptom relapse, personalized follow-up strategies are essential (patient-centered care in fibroid management). This includes regular imaging (ultrasound or MRI) and symptom assessment tailored to the patient's treatment type and reproductive goals. Monitoring helps detect new or recurring fibroids early, optimizing timing for repeat treatment if needed and preserving quality of life.
Personalized Care in Fibroid Management: A Woman-Led Healthcare Approach
What comprehensive obstetrics and gynecology services does a woman-led healthcare provider typically offer?
Women-led healthcare practices specializing in obstetrics and gynecology, particularly those in Queens, NY, often provide a full spectrum of services tailored to the unique needs of women. These services include prenatal care, childbirth support, and postpartum care along with routine gynecological exams. They also address family planning, menopause management, and reproductive health concerns such as uterine fibroids.
In fibroid management, these providers offer personalized treatment plans that may involve medication, minimally invasive procedures, or surgery, depending on symptoms, fibroid size, and reproductive goals. The approach is holistic, focusing on overall wellness and addressing individual concerns to enhance quality of life.
How do patient-centered care models emphasize communication and trust?
Women-led practices excel in creating a patient-first environment where open communication, empathy, and trust are prioritized. This model encourages patients to share their symptoms and preferences freely, allowing healthcare providers to deliver tailored care that aligns with women’s lifestyles and aspirations. This embodies patient-centered care in fibroid management.
How are treatment plans tailored to individual symptoms, reproductive goals, and lifestyle?
Because fibroids and their impact vary widely, treatment is highly individualized. For women wishing to preserve fertility, options like myomectomy or minimally invasive treatments are prioritized. For those with mild or no symptoms, watchful waiting may be advised. Medication choices are carefully selected to control symptoms without compromising future pregnancies. Lifestyle factors and patient preferences are key considerations in decision-making.
What enhanced empathy and understanding do women-led healthcare settings offer?
Women-led healthcare providers often have a deeper understanding of the emotional and physical challenges associated with fibroids and reproductive health. This results in compassionate support that not only treats medical issues but also acknowledges the psychosocial impacts, fostering a stronger therapeutic relationship and improved patient satisfaction. This approach highlights the importance of patient-centered care in fibroid management.
Ensuring Personalized Care: How Woman-Led Providers Tailor Fibroid Treatment
How does a woman-led healthcare provider ensure personalized women's health care?
Woman-led healthcare providers specialize in delivering care that genuinely reflects each woman's unique health journey. By fostering open and trusting communication, they create a safe environment where patients can freely discuss their symptoms, concerns, and treatment preferences without hesitation.
These providers use detailed, comprehensive assessments combined with advanced diagnostic technologies such as transvaginal ultrasound, MRI, and hysterosonography to gain a clear understanding of fibroid size, location, and symptom impact. This thorough evaluation informs highly individualized treatment plans that align with the patient's reproductive goals and lifestyle.
Empathy plays a vital role in recognizing subtle symptoms women may experience but might overlook or underestimate. Woman-led teams are often better attuned to these nuances, providing compassionate listening and validating patient experiences.
Empowerment through education is central to care, as providers engage women in shared decision-making. Patients receive clear, accessible information about all available medical and surgical options, including benefits and possible risks, allowing them to take an active role in their treatment choices.
This personalized, empathetic, and patient-focused approach leads to improved outcomes and higher satisfaction, ensuring that fibroid care respects each woman’s individuality.
Advanced Women's Health Care Options for Fibroid Patients
What advanced women's health care options are available to patients at specialized obstetrics and gynecology centers?
Specialized obstetrics and gynecology centers offer comprehensive and advanced care tailored specifically for women dealing with fibroids and related reproductive health concerns. These centers provide access to cutting-edge diagnostic tools, such as 3D ultrasound and magnetic resonance imaging (MRI), which enhance the precision in identifying fibroid number, size, location, and impact on surrounding uterine structures.
For patients focused on fertility preservation or enhancement, minimally invasive myomectomy options are widely available. These include laparoscopic, robotic-assisted, and hysteroscopic procedures designed to remove fibroids while preserving uterine function and fertility potential. In addition, patients may benefit from in vitro fertilization (IVF) support and other assisted reproductive technologies offered within the integrated care settings.
Moreover, specialized centers commonly benefit from multidisciplinary teams that include gynecologic surgeons, reproductive endocrinologists, interventional radiologists, and maternal-fetal medicine specialists. This collaborative approach ensures high-risk pregnancies complicated by fibroids receive expert management, reducing maternal and fetal risks through personalized monitoring and intervention plans.
State-of-the-art treatment modalities at these centers also involve newer noninvasive and minimally invasive therapies such as MRI-guided focused ultrasound (MRgFUS), uterine artery embolization (UAE), and laparoscopic radiofrequency ablation. In addition, patients may have access to ongoing clinical trials and novel medications aimed at improving symptom control and reducing fibroid recurrence after treatment, providing hope for better long-term outcomes.
These comprehensive services, combining advanced diagnostics with individualized, fertility-sparing, and multidisciplinary care, underscore the immense benefits of specialized obstetrics and gynecology centers for women navigating fibroid treatment and reproductive health challenges.
The Role of Local Specialized Centers in Queens, NY, for Fibroid Management
Access to state-of-the-art fibroid care in Queens, NY
Queens offers women specialized access to advanced fibroid treatment options through clinics affiliated with prominent medical centers like Mount Sinai and collaborations with facilities such as Cleveland Clinic. These centers provide comprehensive diagnostic services including high-quality sonography and MRI, enabling accurate diagnosis and individualized management plans.
Availability of minimally invasive and surgical treatments at local clinics
Patients in Queens benefit from a range of minimally invasive therapies such as uterine artery embolization (UAE), MRI-guided focused ultrasound surgery (FUS), and laparoscopic radiofrequency ablation. Surgical options including myomectomy (both hysteroscopic and laparoscopic/robotic-assisted) and hysterectomy are also available, allowing tailored treatments based on fibroid size, location, and patient fertility desires.
Collaborative and multidisciplinary approach including gynecologists, radiologists, and surgeons
Many Queens-based gynecology centers emphasize a collaborative care model involving board-certified gynecologists, interventional radiologists, and gynecologic surgeons. This team approach ensures patients receive expert evaluation, coordinated treatment strategies, and follow-up, optimizing outcomes and patient safety.
Emphasis on patient comfort, personalized care, and convenience for Queens residents
Local clinics advocate a patient-first philosophy, focusing on personalized care plans that respect individual goals and clinical context. Convenient access within Queens helps reduce treatment delays, while providers emphasize clear communication, thorough counseling, and comfort throughout diagnosis and therapy, enhancing patient experience and adherence.
Emerging Research and Future Directions in Fibroid Treatment
Ongoing Clinical Trials and Advances
Research institutions and medical centers continuously conduct clinical trials for fibroid treatment to improve the safety and efficacy of fibroid treatments. Efforts focus on optimizing existing therapies like uterine artery embolization and magnetic resonance-guided focused ultrasound (MRgFUS), while evaluating long-term outcomes, particularly related to symptom relief and fertility preservation in fibroid treatment.
Novel Medical Treatments with Reduced Side Effects
New hormonal agents, including advanced GnRH antagonists therapy such as relugolix, are being studied to provide symptom control with fewer menopausal-like side effects and less impact on bone density. Additionally, Selective progesterone receptor modulators and other novel compounds are explored to offer targeted fibroid shrinkage with improved safety profiles.
Addressing Health Disparities
Research is increasingly highlighting racial and socioeconomic disparities in fibroid prevalence, severity, and treatment outcomes, especially among African American women (Fibroids in African American women). Future directions emphasize developing equitable access to care, tailoring treatment plans to diverse populations, and reducing barriers to advanced therapies.
Developing Less Invasive and Fertility-Friendly Options
Emerging minimally invasive procedures, including improvements in Laparoscopic radiofrequency ablation and Non-surgical fibroid treatment with FUS, aim to minimize recovery times and preserve uterine integrity. These innovations seek to better support fertility desires while effectively managing fibroid symptoms.
Ongoing innovation in Management of uterine fibroids promises more personalized, effective, and patient-centered care, helping women maintain reproductive potential and quality of life with reduced treatment burdens.
Conclusion: Embracing Tailored Treatment for Effective Fibroid Management
A Personalized Approach to Fibroid Care
Uterine fibroids affect many women but manifest differently for each, emphasizing the necessity of personalized and patient-centered care.
Combining Multiple Treatment Modalities
Effective management often involves integrating medical therapies, minimally invasive procedures, and surgical techniques tailored to individual symptoms, fibroid characteristics, and reproductive goals.
Specialized Centers Enhance Outcomes
Dedicated fibroid centers with expert, woman-led teams provide advanced diagnostics and treatments, ensuring women receive the most appropriate and up-to-date interventions with compassionate support.
Empowering Women Through Knowledge and Options
Informed decision-making empowered by clear information on risks, benefits, and emerging therapies enables women to choose treatments aligning with their lifestyle and fertility plans, ultimately improving health and quality of life.




.png)