Navigating Women's Health: A Comprehensive Guide Across Life Stages

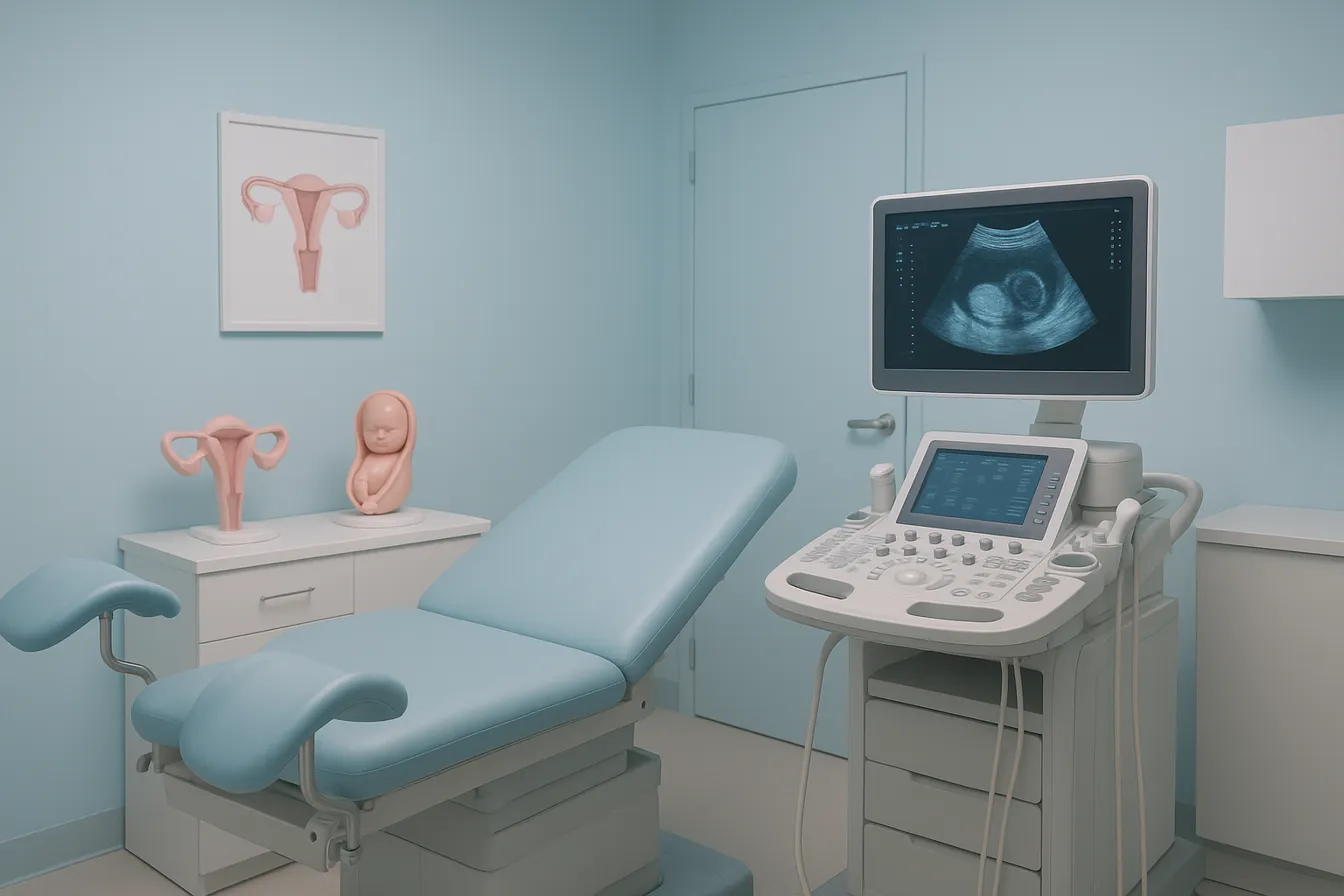
Navigating Pregnancy with Confidence and Care
Overview of Pregnancy Stages
Pregnancy is divided into three trimesters, each with unique developments and care needs.
- First trimester: Crucial for fetal organ and system formation; expect physical and emotional changes like nausea and fatigue.
- Second trimester: Symptoms often improve; the fetus grows in length and weight, and pregnancy becomes more visible.
- Third trimester: Focus on continued fetal growth and preparing the body for childbirth.
Importance of Prenatal Care
Prenatal care includes early and regular checkups starting as soon as pregnancy is suspected.
- Monitors mother and baby’s health through physical exams and medical tests such as blood pressure, blood glucose, and screenings for infections.
- Early detection of complications such as gestational diabetes or preeclampsia helps reduce risks.
- Vaccinations like flu, Tdap, and COVID-19 are recommended to protect mother and baby.
- Prenatal visits also provide guidance on nutrition, exercise, and birth planning.
Healthy Lifestyle Basics During Pregnancy
Maintaining a balanced, nutrient-rich diet supports fetal development and maternal health.
- Include fruits, vegetables, whole grains, lean proteins, and dairy.
- Adequate hydration and prenatal vitamins with folic acid are essential.
- Avoid unsafe foods such as high-mercury fish, raw or undercooked meats, and unpasteurized products.
- Engage in moderate exercise like walking or swimming, pending healthcare provider approval.
- Avoid tobacco, alcohol, drugs, and limit caffeine intake to about 200 mg per day.
- Prioritize sufficient rest, stress management, and regular medical follow-up during pregnancy for best outcomes.
Understanding Pregnancy Trimesters and Fetal Development

Importance of Each Trimester
Pregnancy is divided into three trimesters, each lasting about 13 weeks, playing distinct roles in fetal development and maternal health.
Fetal Organ Formation
The first trimester is crucial as most major body organs and systems of the fetus form during this time. This includes the development of the heart, lungs, brain, and limbs. For more information, see First trimester fetal development.
Symptom Progression Through Trimesters
Early pregnancy symptoms like nausea, morning sickness, and fatigue are most common in the first trimester and usually ease by the second trimester. The second trimester often brings relief from these symptoms, while the third trimester may involve new discomforts as the body prepares for delivery. Visit Second trimester symptom relief for more details.
Growth Milestones of Fetus
During the second trimester, the fetus grows noticeably in length and weight, and organ development continues. The third trimester focuses on rapid growth and weight gain to prepare the baby for birth. Learn more about Third trimester fetal growth.
Overall, understanding these phases helps expectant mothers monitor their health and fetal progress effectively.
The Role of Prenatal Care in Ensuring Maternal and Fetal Health

Early and Regular Prenatal Visits
Prenatal care begins as soon as pregnancy is confirmed and includes scheduled visits typically every four weeks until 28 weeks, then every two weeks until 36 weeks, and weekly thereafter until delivery. These early and regular prenatal care visits allow healthcare providers to monitor the mother's and baby's health, detect potential complications early, and offer guidance tailored to individual needs.
Key Medical Tests During Pregnancy
Throughout pregnancy, several medical tests during pregnancy are conducted to ensure both maternal and fetal well-being. Routine blood and urine tests screen for Rh factor testing, hepatitis B screening, urinary tract infection testing, syphilis test, HIV screening, rubella immunity, and Group B strep test. Prenatal screening tests such as ultrasounds assess fetal development and estimate the due date. Between 24 and 28 weeks, all pregnant women undergo screening for gestational diabetes testing to prevent complications.
Monitoring Maternal Conditions Like Gestational Diabetes and Preeclampsia
Blood pressure monitoring is regularly monitored to detect preeclampsia signs, a pregnancy-related high blood pressure condition. Gestational diabetes testing helps to identify and manage elevated blood sugar during pregnancy, reducing risks for both mother and baby. Early detection through testing enables timely interventions to promote a healthy pregnancy.
Screening Protocols for Infections and Risk Factors
Prenatal care includes comprehensive infection screening to prevent transmission to the fetus and reduce complications. Vaccinations during pregnancy, such as those for flu vaccine during pregnancy and whooping cough, are recommended during pregnancy to protect mother and baby. Pregnant women are advised to avoid harmful substances and take precautions against infections like preventing Zika virus infection. Sharing family health history and pregnancy helps guide additional screening and care.
These tailored prenatal care steps are essential for safeguarding the health of mothers and their babies throughout pregnancy, ensuring positive outcomes through early detection and appropriate management.
Nutrition Essentials and Appropriate Weight Gain During Pregnancy

Nutrient Requirements Including Folic Acid, Iron, Calcium
During pregnancy, specific nutrients become essential to support both maternal health and fetal development. Folic acid intake is critical, with recommendations of about 600 micrograms daily during pregnancy to help prevent neural tube defects. Iron needs increase to approximately 30 mg per day, supporting the increased blood volume and preventing anemia. Calcium is similarly vital to aid in building the baby’s bones and teeth, with good dietary sources including low-fat dairy products, dark green vegetables, and fortified foods.
Healthy Balanced Diet Recommendations
A healthy pregnancy diet should be well-rounded, rich in fruits, vegetables, whole grains, lean proteins, and low-fat dairy products. Including sources of healthy fats such as nuts, seeds, and fatty fish low in mercury also supports fetal brain and tissue development. Caloric intake increases moderately, particularly in the second and third trimesters—by about 340 and 450 extra calories daily, respectively. For more healthy pregnancy tips, consult reliable sources.
Weight Gain Guidelines by Pre-Pregnancy BMI
Recommended pregnancy weight gain depends on a woman's pre-pregnancy body mass index (BMI):
| Pre-Pregnancy BMI | Recommended Weight Gain | Notes |
|---|---|---|
| Underweight | 28-40 pounds | Supports healthy fetal growth |
| Healthy weight | 25-35 pounds | Preferred range for most pregnancies |
| Overweight | 15-25 pounds | Reduces risk of complications |
| Obesity | 11-20 pounds | Lower gain recommended for improved outcomes |
Weight gain should be gradual, especially during the first trimester (1-4 pounds), followed by 2 to 4 pounds per month until delivery. For detailed healthy weight gain during pregnancy information, visit trusted health resources.
Foods to Avoid and Supplementation
Certain foods should be avoided during pregnancy due to risks of foodborne illness or harmful substances. These include high-mercury fish (king mackerel, shark, swordfish), unpasteurized dairy products, raw or undercooked meats and eggs, deli meats, and raw sprouts. Prenatal vitamins, particularly those containing folic acid, iron, and calcium, are recommended to fill nutritional gaps and promote healthy pregnancy outcomes. For guidance on foods to avoid during pregnancy and prenatal supplementation, refer to established medical guidelines.
Following these nutrition and weight gain guidelines supports the health and well-being of both mother and baby throughout pregnancy.
Safe Exercise, Rest, and Lifestyle Habits to Support Pregnancy Wellness

Recommended Physical Activities
Engaging in physical activity recommendations for pregnant women is beneficial for both the mother and the baby. Activities such as walking, swimming, prenatal yoga, and water aerobics are safe choices that can help reduce common pregnancy discomforts like backaches, leg cramps, and bloating. Most pregnant women are encouraged to aim for at least 150 minutes of moderate-intensity aerobic activity per week, but always with prior approval from their healthcare provider to ensure safety.
Importance of Hydration and Sleep
Hydration and exercise in pregnancy by drinking 8 to 10 cups of water daily supports increased blood volume, amniotic fluid levels, and helps prevent common issues such as constipation and swelling. Adequate rest is equally crucial; pregnant women should aim for 7 to 9 hours of sleep per night, using comfortable positions such as sleeping on the left side with appropriate pillow support to improve circulation and comfort.
Stress Management Techniques
Managing stress is an important aspect of pregnancy wellness. Techniques like deep breathing exercises, meditation, prenatal yoga, and seeking social support from family or support groups can help reduce anxiety and promote emotional balance. Adequate sleep and planned relaxation contribute significantly to maintaining mental health during pregnancy.
Avoiding Harmful Substances and Environmental Risks
Pregnant women should avoid alcohol, tobacco, recreational drugs, and limit caffeine intake to about 200 milligrams daily. Exposure to harmful chemicals, toxic substances, and infectious agents should be minimized by practicing good hygiene and safe food preparation. Avoiding high-risk activities like hot tubs, heavy lifting, and contact sports is also advised to protect maternal and fetal health by avoiding harmful substances in pregnancy.
Vaccinations, Infection Prevention, and Managing Illness During Pregnancy
Recommended Vaccines During Pregnancy
Pregnant women are strongly advised to receive certain vaccines that protect both mother and baby. The flu vaccine during pregnancy is recommended annually during flu season as it contains no live virus and effectively reduces flu-associated complications. The whooping cough vaccine (Tdap vaccine, which protects against tetanus, diphtheria, and pertussis) is also recommended during pregnancy to safeguard newborns against whooping cough. Additionally, COVID-19 vaccination during pregnancy is highly encouraged as pregnant women face a higher risk of severe illness from COVID-19; vaccination during pregnancy, breastfeeding, or when planning pregnancy is safe and effective.
Vaccines to Avoid
Certain vaccines containing live, attenuated viruses should be avoided during pregnancy. These include the nasal spray flu vaccine, the MMR vaccine (measles, mumps, rubella), and the chickenpox vaccine due to the potential risk to the fetus. For detailed guidance, see Vaccines to avoid during pregnancy.
Infection Prevention Strategies
Preventing infection is crucial during pregnancy. Good hygiene practices such as frequent handwashing, safe food handling, and avoiding exposure to infections like the Zika virus are important. Pregnant women should avoid consumption of unpasteurized dairy products and undercooked or raw meats and seafood to prevent foodborne illness. Additionally, avoiding contact with rodents and practicing safe sex reduce the risk of infections that can negatively affect pregnancy. For comprehensive guidance, refer to Infection prevention in pregnancy.
Managing Common Illnesses and COVID-19 Risks
Flu and COVID-19 are significant concerns during pregnancy. Pregnant women should seek advice from healthcare providers for proper management if illness occurs. Vaccinations help minimize risks. Avoidance of smoking and harmful substances and monitoring for warning signs such as high fever or breathing difficulties enable early intervention. Managing flu during pregnancy and COVID-19 vaccination for pregnant women remain especially critical as pregnancy increases susceptibility to severe outcomes.
These measures collectively contribute to a safer pregnancy by reducing infection risks and protecting both maternal and fetal health.
Tailored Prenatal Care and Addressing Social Determinants of Health
What is personalized prenatal care?
Personalized prenatal care means tailoring pregnancy care plans to meet the unique medical, social, and emotional needs of each individual. Healthcare providers work with pregnant persons to understand their preferences, risks, and circumstances, creating a care schedule and services that best support their health and wellbeing.
How do telemedicine and flexible visit schedules help?
Flexible prenatal care may include fewer or more prenatal visits based on an individual's risk level. Telemedicine in prenatal care allows remote appointments, which can improve accessibility, reduce travel burdens, and enhance convenience. These options make it easier for those with limited transportation or time constraints to receive consistent monitoring and advice.
Why is screening for social needs important?
Assessing social determinants of health—such as housing stability, food security, and transportation access—before 10 weeks gestation helps identify barriers that could affect pregnancy outcomes. Supporting pregnant individuals through referrals and community resources ensures comprehensive care that extends beyond medical needs. This is a key component of tailored prenatal care delivery.
What role does shared decision-making and culturally sensitive care play?
Shared decision-making respects the pregnant person's values and choices in care plans. Incorporating culturally humble and trauma-informed approaches fosters trust and improves engagement. This respectful collaboration helps address disparities and results in better health experiences and outcomes.
Preparing for Labor, Delivery, and Postpartum Recovery
Birth Planning and Pain Management Options
Creating a birth plan allows expectant mothers to communicate their preferences for labor and delivery, including Childbirth pain relief options such as epidurals, breathing techniques, or medications. Discussing these choices with healthcare providers can empower women to make informed decisions and foster a positive birth experience.
Importance of Pelvic and Mental Health Monitoring Post-Birth
After delivery, monitoring Gynecological care is crucial to detect and manage physical changes or complications. Additionally, Mental health conditions in pregnancy checkups help identify conditions like postpartum depression, anxiety, or mood shifts, allowing timely intervention and support for a healthier recovery.
Support Systems and Breastfeeding Guidance
Support from family, friends, and healthcare professionals plays a vital role in planning postpartum care. Breastfeeding preparation guidance from lactation consultants or classes can ease the learning process, promote bonding, and provide lasting health benefits for both mother and baby.
Postpartum Depression Awareness
Awareness and education about postpartum care planning are essential, as many women experience emotional challenges after childbirth. Recognizing symptoms early and seeking treatment or counseling can greatly improve outcomes and support the mother's overall health.
High-Risk Pregnancies: Specialized Care and Managing Complications
What Are Common Conditions in High-Risk Pregnancies?
High-risk pregnancies may involve conditions such as gestational diabetes testing, hypertension (including preeclampsia signs), and Pregnancy and delivery considerations for twins and triplets. These situations require extra attention due to potential risks for both mother and baby.
How Is Specialized Monitoring Implemented?
Women with high-risk pregnancies receive Tailored prenatal care delivery, which includes more frequent prenatal visits and specialized tests. Monitoring involves regular blood pressure monitoring during pregnancy to detect hypertension, gestational diabetes testing between 24 and 28 weeks, and Fetal growth and health monitoring.
Advanced care may utilize digital tools such as remote monitoring devices to track vital signs like blood sugar and blood pressure in real-time. Such monitoring helps promptly identify complications and allows for timely interventions.
What Treatment Protocols Are Followed?
Managing high-risk conditions includes strict control of blood sugar for gestational diabetes and blood pressure for hypertensive disorders, often requiring medication adjustments under medical supervision. Nutritional counseling and lifestyle modifications, including appropriate diet and physical activity, play crucial roles.
Pregnancy and delivery considerations for twins and triplets often necessitate individualized nutritional and delivery planning to support fetal growth and reduce premature birth risks.
How Do Healthcare Providers Support High-Risk Pregnant Women?
Counseling addresses emotional well-being by reassuring women that with specialized care, a healthy pregnancy and delivery are possible even with complications. Providers offer clear information about the condition, available treatments, and implications for labor and postpartum care.
Support also includes preparing creating a birth plan that accommodate specific risks and fostering open communication for shared decision-making. Mental health screening and support for anxiety and depression are integral components of comprehensive care.
Prioritizing individualized care enhances outcomes and empowers women throughout their pregnancy journey.
The Importance of Mental Health and Emotional Well-being Throughout Pregnancy
Recognizing Prenatal and Postpartum Depression and Anxiety
Pregnancy can bring a range of emotions, but it also raises risks for mental health conditions in pregnancy like depression and anxiety, both before and after birth. Common signs include persistent sadness, excessive worry, mood swings, and difficulty sleeping. Awareness of these symptoms is crucial for timely support and treatment.
Accessing Counseling and Support
Women experiencing mental health challenges during pregnancy or postpartum should seek professional counseling options. Healthcare providers often recommend therapy tailored for pregnant or new mothers, which can include individual counseling, support groups, or specialized maternal mental health services. Early intervention enhances recovery and promotes healthier outcomes for both mother and child.
Stress Reduction Techniques and Community Resources
Managing stress is an important part of emotional well-being during pregnancy. Techniques such as prenatal yoga, meditation, and deep breathing exercises can alleviate anxiety and improve mood. Community resources, including peer support groups and maternal health organizations, provide valuable social connection and guidance. Family support also plays a key role in coping with pregnancy changes and postpartum adjustment.
Empowering Expectant Mothers for Optimal Health Outcomes
Recap of Pregnancy Care Principles
A healthy pregnancy begins with early and regular prenatal care, which includes routine checkups and essential screenings to monitor the health of both mother and baby. Nutritional support through a balanced diet and prenatal vitamins, especially folic acid, plays a vital role in fetal development and prevents birth defects.
Vaccinations such as the flu and COVID-19 vaccines are recommended to protect against infections that can complicate pregnancy. Equally important is avoiding harmful substances like tobacco, alcohol, and certain medications, while maintaining safe physical activity.
Early Prenatal Engagement Encouraged
Expectant mothers are encouraged to initiate prenatal care as soon as pregnancy is suspected. Early engagement ensures timely medical guidance, relevant testing, and a foundation for healthy lifestyle choices throughout pregnancy.
This proactive approach helps identify risks early and supports better pregnancy outcomes by addressing health conditions, nutrition, and vaccination needs promptly.
Personalized, Compassionate Care
Tailored prenatal care respects individual needs, preferences, and social circumstances, enhancing accessibility and patient experience. Compassionate care provided by healthcare professionals fosters trust, emotional well-being, and informed decision-making.
Supportive communication and attention to mental health are essential components that empower women to navigate pregnancy confidently and advocate for their health and their baby’s.
By embracing these principles, expectant mothers can optimize their health and enjoy a positive pregnancy journey.




.png)