Navigating Women's Health: A Comprehensive Guide Across Life Stages
Understanding Ovarian Cysts: The Role of Imaging
Overview of Ovarian Cysts
Ovarian cysts are fluid-filled sacs that develop on or within the ovaries and are common in women, especially during reproductive years. Most cysts are benign and often resolve without treatment. Functional cysts, linked to the menstrual cycle, are the most frequent type, while other cysts include dermoid cysts, endometriomas, and cystadenomas.
Importance of Imaging in Diagnosis
Imaging plays a crucial role in accurately detecting and characterizing ovarian cysts. It helps determine the cyst's size, location, and nature—whether solid or fluid-filled—which guides management decisions and early intervention when necessary. Proper imaging is especially vital for evaluating cysts in postmenopausal women, where the risk of malignancy is higher.
Basic Imaging Modalities Used
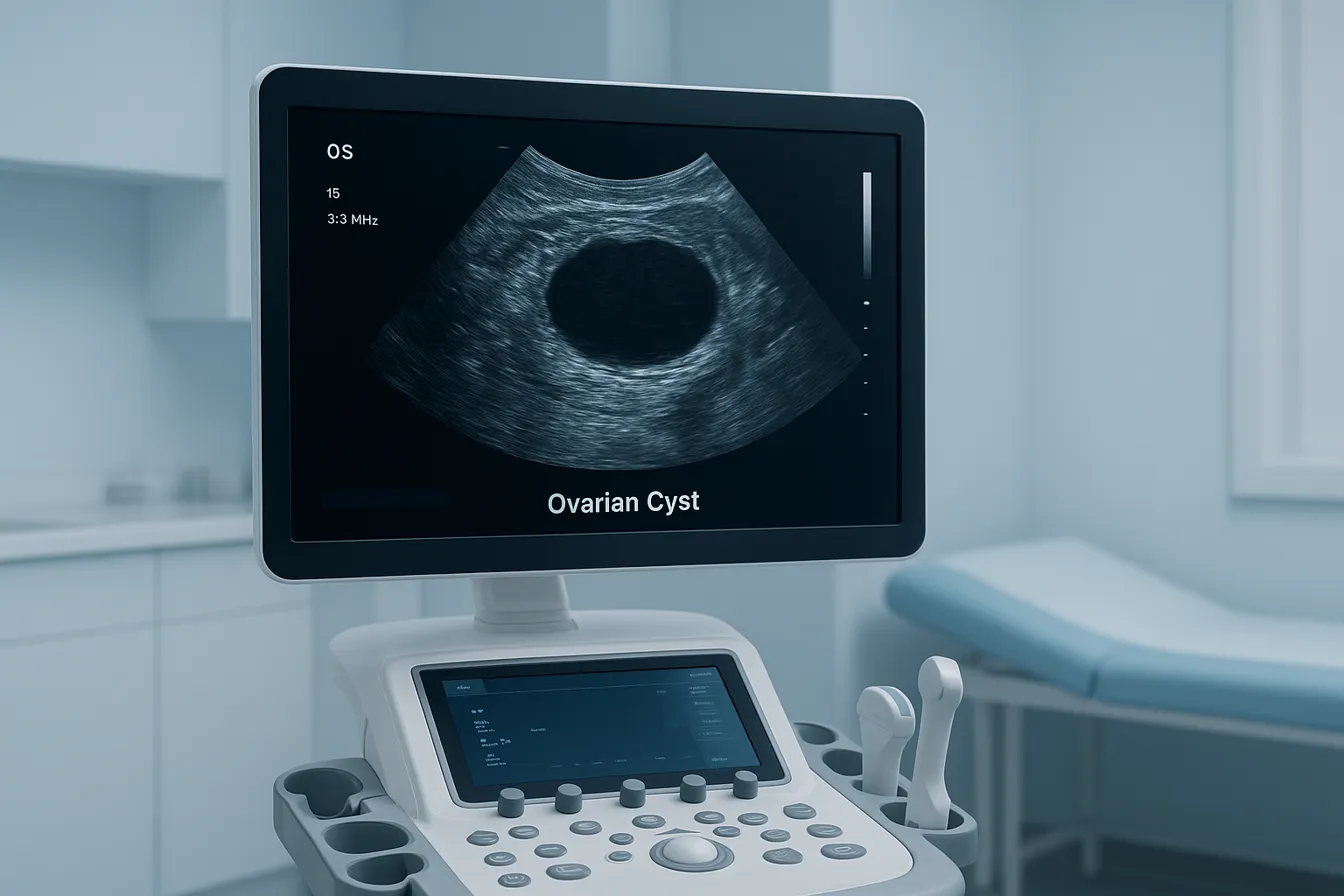
Pelvic ultrasound is the primary and most accessible imaging technique, often performed transvaginally. It uses high-frequency sound waves to create clear images of the ovaries and uterus. Ultrasound assesses cyst size, composition, and associated features like septations or blood flow. In more complex cases, additional imaging such as MRI may be employed to provide enhanced soft tissue contrast or further evaluate indeterminate lesions, while CT scans are less commonly used due to radiation exposure concerns, especially in pregnancy.
This imaging-based approach ensures accurate diagnosis, risk assessment, and personalized care for women with ovarian cysts.
Key Facts on Ovarian Cyst Diagnosis and Imaging Techniques
- Ultrasound, especially transvaginal, is the primary tool for ovarian cyst evaluation.
- Ultrasound features help differentiate simple, hemorrhagic, endometriomas, dermoid, and complex cysts.
- Color Doppler ultrasound assesses blood flow, aiding in benign vs. malignant cyst differentiation.
- Size and morphology thresholds guide follow-up and management, with specific criteria for pre- and postmenopausal women.
- MRI is used for further characterization of indeterminate or complex cysts, using T1, T2, fat-saturation, and DWI sequences.
- CT scans are mainly utilized for staging and complication assessment in confirmed or suspected malignancies.
- MRI can identify hemorrhagic content and fat in cysts, aiding in benign vs. malignant distinction.
- Ultrasound remains the initial choice due to high resolution and accessibility, with MRI and CT reserved for complex cases.
- Limitations of advanced imaging include cost, availability, radiation (CT), and patient contraindications.
- Using combined modalities ensures accurate diagnosis, risk stratification, and appropriate management of ovarian cysts.
1. Pelvic Ultrasound: The Primary Tool for Ovarian Cyst Evaluation
What imaging technique is primarily used to diagnose ovarian cysts?
Pelvic ultrasound for ovarian cysts is the primary and most effective imaging technique for diagnosing ovarian cysts. This includes both transvaginal ultrasound and transabdominal ultrasound methods, with transvaginal ultrasound offering superior resolution for evaluating cyst details due to the proximity of the probe to the ovaries. Ultrasound uses high-frequency sound waves captured by a transducer to create images of the uterus and ovaries. This allows clinicians to confirm cyst presence, precise location, size, and composition — whether fluid-filled (cystic) or solid.
Use of transvaginal versus transabdominal ultrasound techniques
Transvaginal ultrasound involves inserting a probe into the vagina, providing clearer and more detailed images for small or complex cysts, especially in premenopausal women. Transabdominal ultrasound is performed over the lower abdomen and is useful for larger masses or when the transvaginal approach is not feasible. Both techniques complement each other, with transvaginal ultrasound commonly preferred for initial detailed evaluation.
Ultrasound features distinguishing cyst types
Ultrasound helps differentiate cyst types by their distinct appearances:
- Simple cysts: Anechoic (dark), unilocular, thin smooth walls, no internal septations or solid components, and show posterior acoustic enhancement.
- Hemorrhagic cysts: Present with complex cystic masses containing internal echoes (due to blood), often without internal vascular flow.
- Endometriomas: Homogeneous, hypoechoic with diffuse low-level internal echoes, often described as 'ground-glass' appearance.
- Dermoid cysts (mature cystic teratomas): Characteristic fat-fluid levels, calcifications, and hyperechoic nodules causing shadowing ('tip of the iceberg' sign).
- Complex or solid cysts: Presence of thick, irregular walls, septations, solid areas, papillary projections, or increased blood flow suggests suspicion for malignancy.
References for these features can be found in Ultrasound features to categorize adnexal masses and Ultrasound assessment of ovarian lesions.
Role of Doppler ultrasound in blood flow assessment
Color Doppler ultrasound assesses blood flow within ovarian cysts and surrounding tissues. Benign simple cysts typically lack internal vascularity. Increased blood flow, especially in solid areas or septations, can indicate neovascularization associated with malignancies. Corpus luteal cysts may show the characteristic 'ring of fire' pattern with increased peripheral blood flow but are benign.
Size and morphology criteria for benign and suspicious cysts
- Size thresholds:
- Premenopausal women: Simple cysts ≤3 cm are usually physiological follicles and typically do not require follow-up. Cysts >3 cm are recorded with follow-up recommendations depending on size and characteristics.
- Postmenopausal women: Simple cysts ≤1 cm are generally considered insignificant without follow-up. Cysts >3 cm should be closely monitored.
- Morphologic features: Simple cysts with thin, smooth walls and no septations or solid components are generally benign. Features raising suspicion include multilocularity, papillary projections, thick septations (≥3 mm), ascites, lymphadenopathy, or peritoneal deposits.
These criteria are elaborated in Ultrasound for ovarian cyst evaluation and Ultrasound for ovarian cysts.
Follow-up protocols based on ultrasound findings
Follow-up ultrasound schedules are tailored based on cyst size, morphology, and menopausal status:
- Premenopausal women:
- Cysts >3-5 cm but <7 cm generally warrant ultrasound follow-up in 2-6 months.
- Cysts >7 cm may require more frequent monitoring or surgical evaluation.
- Postmenopausal women:
- Cysts between 3-5 cm often require follow-up imaging within 6-12 months along with tumor marker assessment (e.g., CA 125 testing).
- Larger or complex cysts usually prompt specialist referral and possible surgical intervention.
Most simple cysts in premenopausal women resolve spontaneously within a few months and carry a low risk of malignancy. In contrast, solid or complex cysts, especially postmenopause, demand thorough evaluation to rule out cancer. For further information on follow-up, see the SRU Consensus Conference on adnexal cysts and Ovarian cyst risk assessment and surgical referral.
Ultrasound with Doppler remains indispensable for early detection and risk stratification of ovarian cysts, guiding appropriate clinical management and optimizing patient outcomes. More on Diagnosis and Management of Ovarian Cysts.
2. Advanced Imaging: MRI and CT in Complex and Indeterminate Cases

When are MRI and CT scans used for ovarian cyst evaluation?
Magnetic Resonance Imaging (MRI) and Computed Tomography (CT) play important complementary roles in the assessment of ovarian cysts, especially in cases where ultrasound features of simple cysts are complex or inconclusive.
MRI is typically reserved for further characterization of indeterminate or complex ovarian lesions detected on ultrasound. It offers detailed soft tissue contrast that helps clarify the nature of cyst contents and the cyst’s morphology. Conversely, CT scans are mainly utilized in the staging of confirmed malignant ovarian cysts and to evaluate complications such as hemorrhagic cyst rupture or metastasis.
What MRI protocols and sequences are useful in cyst characterization?
MRI protocols for ovarian lesion assessment usually include multiple sequences to enhance lesion characterization:
- T2-weighted sequences: Highlight fluid-filled structures and differentiate cystic from solid components.
- T1-weighted sequences: Detect substances like blood or fat within lesions.
- Fat-saturated sequences: Suppress fat signal to better identify fatty components typical of dermoid cysts.
- Diffusion-weighted imaging (DWI): Helps assess cellular density and may assist in distinguishing benign from malignant lesions.
These sequences allow precise identification of features such as hemorrhagic content within cysts or fat components in teratomas, improving diagnostic accuracy beyond what ultrasound can offer.
How is CT scanning used in the context of ovarian cysts?
CT imaging is commonly applied for patients with confirmed or suspected ovarian malignancies to evaluate the extent of disease involvement, assess for lymphadenopathy, peritoneal implants, or distant metastases.
It is also valuable in emergency situations to detect complications like hemorrhagic cyst rupture or to evaluate hemoperitoneum. However, CT provides less soft tissue contrast compared to MRI and is generally not utilized for initial cyst characterization.
Examples of features distinguishable by MRI
MRI can identify specific characteristics within ovarian cysts that aid in diagnosis:
- Hemorrhagic cysts: Blood products exhibit high signal intensity on T1-weighted images.
- Mature cystic teratomas (dermoid cysts): Fat within the cyst appears bright on T1-weighted images and loses signal on fat-suppressed sequences. Calcifications and Rokitansky nodules can also be seen.
By detailing the internal composition, MRI helps differentiate benign cysts from those potentially malignant or complex, influencing Diagnosis and Management of Ovarian Cysts.
Complementary use of MRI and CT to ultrasound findings
Ultrasound for ovarian cyst evaluation remains the first-line imaging modality for ovarian cyst detection and initial evaluation due to its accessibility and high resolution for pelvic anatomy.
MRI is used when ultrasound is inconclusive or for further assessment of complex cysts, providing superior soft tissue contrast and content identification.
CT complements these modalities mainly for staging malignancies or evaluating complications, especially in acute settings.
Limitations and considerations of advanced imaging modalities
MRI and CT, despite their benefits, are more costly and less accessible than ultrasound. MRI’s longer scan times and contraindications for some patients (e.g., those with certain implants) must be considered.
CT involves radiation exposure, limiting its use particularly in pregnancy.
Both modalities require careful interpretation by experienced radiologists specialized in gynecologic imaging to optimize clinical utility.
| Imaging Modality | Primary Use | Key Strengths | Limitations |
|---|---|---|---|
| Ultrasound | Initial cyst detection and follow-up | Real-time imaging, no radiation | Operator dependent, limited in complex cases |
| MRI | Characterization of complex/indeterminate cysts | Superior soft tissue contrast, no radiation | Expensive, patient contraindications, availability |
| CT | Staging malignancy, evaluating complications | Fast, effective for assessing metastasis and hemorrhage | Radiation exposure, limited soft tissue detail |
Advanced imaging, particularly MRI and CT, plays a crucial role in the assessment of ovarian cysts when ultrasound findings are insufficient, helping tailor appropriate management strategies with greater diagnostic confidence.
The Critical Role of Imaging in Effective Ovarian Cyst Management
Imaging Techniques Used in Ovarian Cyst Diagnosis
Ultrasound remains the first and most crucial imaging modality for ovarian cysts. Transvaginal ultrasound provides detailed images of the ovary, helping identify cyst size, location, and whether it is fluid-filled or solid. This modality also assesses features such as wall thickness, septations, and vascular blood flow using Doppler studies.
In cases where ultrasound results are inconclusive or cyst features suggest complexity, MRI offers superior soft tissue contrast aiding in differentiating benign from malignant lesions. CT scans are less commonly used but can evaluate complications like hemoperitoneum or metastasis when malignancy is suspected.
Impact on Patient Care and Treatment Planning
Accurate imaging allows clinicians to classify cysts effectively—simple cysts often warrant watchful waiting, while complex cysts may require surgical evaluation. Tumor marker tests, particularly CA 125, complement imaging results to assess cancer risk, especially in postmenopausal women.
Minimally invasive laparoscopic surgery can be planned based on imaging, preserving ovarian function when possible. Imaging findings also guide the frequency and timing of follow-up evaluations to monitor cyst evolution or resolution.
Importance of Regular Monitoring, Especially Postmenopause
In postmenopausal women, imaging surveillance is essential because ovarian cysts have a higher risk of malignancy. Simple cysts below certain size thresholds may not require follow-up, but larger or complex cysts necessitate regular ultrasounds and sometimes tumor marker evaluations to facilitate early detection of malignancy. Such vigilance improves patient outcomes by ensuring timely and appropriate management.
Overall, precise imaging techniques underpin effective ovarian cyst diagnosis, risk assessment, and tailored patient care.




.png)