Navigating Women's Health: A Comprehensive Guide Across Life Stages

Understanding the Importance of Prenatal Care
Definition of Prenatal Care
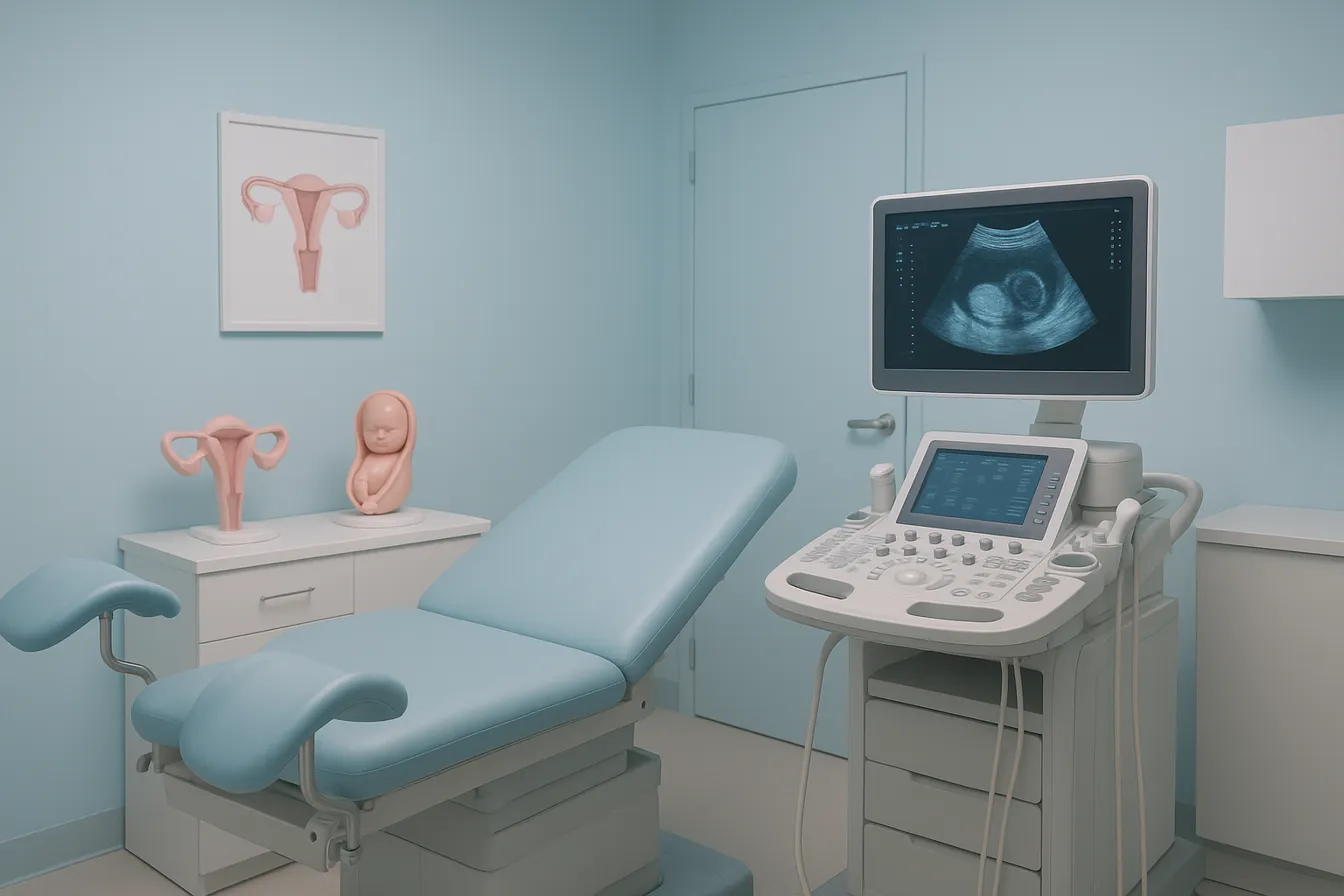
Prenatal care involves regular medical visits during pregnancy to monitor the health of both mother and baby. It includes physical exams, lab tests, ultrasounds, and guidance on nutrition and lifestyle.
Importance of Early and Regular Prenatal Visits
Starting prenatal care early in pregnancy is crucial for identifying and managing potential health risks. Routine visits allow healthcare providers to monitor fetal development, screen for complications like gestational diabetes or preeclampsia, and provide timely interventions.
Role of Prenatal Care in Maternal and Fetal Health
Prenatal care supports maternal well-being by advising on nutrition, exercise, and managing common pregnancy symptoms. It ensures fetal health through monitoring growth and oxygen supply. Early detection of issues improves outcomes for both mother and baby.
Local Context for Queens, NY Patients
Women in Queens can access comprehensive prenatal services through local hospitals and clinics, such as NYC Health + Hospitals/Queens and NewYork-Presbyterian Queens. These centers offer culturally sensitive care, advanced ultrasonography, and support programs tailored to community needs, ensuring personalized and accessible obstetric care.
Key Facts on Pregnancy Nutrition, Exercise, and Monitoring
- Pregnancy’s nutritional requirements include folic acid, iron, calcium, vitamin D, choline, and omega-3 fatty acids to support mother and fetus.
- Pregnant women should avoid unpasteurized dairy, high-mercury fish, raw meats, and limit caffeine to reduce health risks.
- Healthy pregnancy weight gain varies by pre-pregnancy BMI, with 25-35 lbs for normal weight women, monitored with healthcare guidance.
- Exercise during pregnancy is safe and beneficial, with at least 150 minutes of moderate activity weekly, including walking, swimming, and prenatal yoga.
- Activities like contact sports, high-impact or risky activities, and exercise in high heat should be avoided during pregnancy.
- Signs like vaginal bleeding, severe pain, dizziness, or decreased fetal movement require immediate medical attention.
- Postpartum recovery involves managing bleeding, pain relief, supporting pelvic health, and using breastfeeding supplies, with mental health support.
- Uterine and fetal monitoring through ultrasound, external, and internal fetal monitoring ensures ongoing maternal and fetal health.
- Comprehensive obstetrical services in Queens, NY, include prenatal care, high-risk management, labor, delivery, and postpartum support.
- Routine prenatal screenings include blood pressure, gestational diabetes tests, and infection screenings, with ultrasounds for fetal health assessment.
1. Optimizing Nutrition for Mother and Baby
What are the key nutritional requirements during pregnancy?
Pregnancy increases the body's nutritional demands to support both mother and baby's health. Starting in the second trimester, calorie needs rise by approximately 340 extra calories daily for a single baby, with higher allowances for twins or multiples. Essential vitamins and minerals include:
- Folic acid: 600 micrograms daily to help prevent neural tube defects, recommended before conception and through the first trimester.
- Iron: 27 mg daily to support the increased blood volume and aid fetal growth; found in lean meats, beans, and fortified cereals.
- Calcium: 1,000 to 1,300 mg daily depending on maternal age to strengthen fetal bones and teeth, sourced from dairy and leafy greens.
- Vitamin D: 600 IU daily, essential for calcium absorption, with supplementation as needed.
- Choline: 450 mg daily, critical for fetal brain development, found in eggs, milk, and meat.
- Omega-3 fatty acids: From low-mercury fish, supporting brain development; recommended two to three servings per week.
In addition to these, maintaining a balanced diet incorporating fruits, vegetables, whole grains, lean proteins, and low-fat dairy is vital. Hydration is equally important, with an advised intake of 8-12 cups of fluids daily.
What foods should pregnant women avoid?
Certain foods can pose risks during pregnancy and should be limited or avoided to protect both mother and baby:
- Unpasteurized milk products and soft cheeses unless made from pasteurized milk.
- Raw or undercooked fish, meats, and eggs, which may carry infections.
- Deli meats and hot dogs unless thoroughly heated.
- Refrigerated pâté, meat spreads, and smoked seafood.
- Fish high in mercury levels such as shark, swordfish, king mackerel, tilefish, marlin, and orange roughy should be avoided.
- Caffeine should be limited to under 200 mg daily.
- Alcohol consumption should be completely avoided during pregnancy.
How should weight gain be managed during pregnancy?
Healthy weight gain varies based on pre-pregnancy body mass index (BMI):
| Pre-Pregnancy BMI | Recommended Weight Gain (lbs) | Purpose |
|---|---|---|
| Underweight (BMI <18.5) | 28-40 | Support fetal development |
| Normal weight (BMI 18.5-24.9) | 25-35 | Balance fetal and maternal health |
| Overweight (BMI 25-29.9) | 15-25 | Minimize excess maternal fat gain |
| Obese (BMI ≥30) | 11-20 | Reduce risk of complications |
Pregnant women should work with healthcare providers to monitor gain and adjust nutrition plans accordingly. Following these guidelines promotes optimal fetal growth while supporting maternal health throughout pregnancy.
2. Safe and Effective Exercise Practices During Pregnancy
Is exercise safe during pregnancy and what are the recommendations?
Exercise during pregnancy is safe and highly beneficial for women who have uncomplicated pregnancies. It is recommended to engage in at least 150 minutes of moderate-intensity aerobic activity per week. This can be broken down into shorter sessions, such as 30 minutes on five days each week, allowing flexibility for daily routines. Safe activities include walking, swimming, stationary cycling, and modified yoga or Pilates, all of which support cardiovascular health, muscle strength, and stress reduction.
Regular physical activity helps lower the risk of gestational diabetes, preeclampsia, excessive weight gain, and cesarean deliveries. It also aids in easing common pregnancy discomforts such as back pain and constipation, and promotes better postpartum recovery.
What types of exercise should be avoided during pregnancy?
Certain activities pose risks during pregnancy and should be avoided. These include contact sports (e.g., soccer, kickboxing), high-impact or high-fall-risk activities like skiing or horseback riding, scuba diving, skydiving, and any exercise that involves rapid altitude changes. Hot yoga and exercises in high heat and humidity are discouraged to prevent overheating.
Importantly, pregnant women should avoid lying flat on their backs after the first trimester, as this position can reduce blood flow to the uterus.
Recommended Types of Exercise and Intensity Levels
- Walking: Low impact, easy to adjust pace.
- Swimming and water aerobics: Reduce strain on joints and alleviate back pain.
- Stationary cycling: Safe cardiovascular workout without risk of falls.
- Prenatal yoga and Pilates: Enhance flexibility and core strength with modifications.
Women who were active with vigorous exercises before pregnancy may continue with their routines, but should consult their healthcare provider.
Guidelines on Duration and Frequency
- Aim for 150 minutes of moderate aerobic activity weekly.
- Break into sessions (e.g., 30 minutes, 5 days a week).
- Gradually increase duration and intensity as tolerated.
Precautions and Contraindications
Women with medical or obstetric complications such as placental issues, severe anemia, heart or lung diseases, preeclampsia, or bleeding should seek medical advice before exercising. Routine bed rest is generally not advised.
Signs to Stop Exercising
Exercise should be immediately stopped if any of these occur:
- Vaginal bleeding
- Dizziness or faintness
- Severe abdominal pain
- Chest pain or shortness of breath
- Muscle weakness or calf pain/swelling
- Uterine contractions or decreased fetal movements
Postpartum Exercise Importance
Physical activity after childbirth greatly supports recovery, helps manage weight, improves mood, and lowers the risk of postpartum depression. Postpartum exercise should start gently, with activities like walking and pelvic floor exercises (e.g., Kegels), gradually increasing based on individual recovery.
Healthcare providers in Queens, NY encourage pregnant and postpartum women to incorporate safe exercise routines into their care plan to promote overall women’s health and well-being.
3. Monitoring and Support Throughout Pregnancy and Postpartum
What monitoring methods are used to ensure fetal and maternal health?
Electronic fetal monitoring methods plays a vital role during pregnancy and labor by tracking the baby’s heart rate and contractions. External monitoring is done using ultrasound sensors placed on the mother's belly, while internal monitoring involves a sensor attached to the baby’s scalp during labor after the cervix has dilated. This allows healthcare providers to assess if the baby is receiving enough oxygen and to identify any distress.
Regular prenatal screenings and tests are essential components of comprehensive pregnancy care. These include blood pressure checks to detect preeclampsia, screening for gestational diabetes typically performed between 24 and 28 weeks, and tests for infections such as Group B strep, syphilis, and HIV. Ultrasounds are used to monitor fetal growth and placental health. Early screening helps identify risks and promotes timely interventions for a healthy pregnancy.
What signs and symptoms warrant immediate medical attention?
Pregnant women should promptly consult their healthcare provider if they experience warning signs such as vaginal bleeding, severe abdominal pain, dizziness, chest pain, sudden swelling, decreased fetal movement, or contractions before term. These symptoms may indicate complications requiring urgent assessment and management to protect maternal and fetal health.
What postpartum care essentials support recovery and wellbeing?
Postpartum essentials are crucial during the first 12 weeks after delivery, a time when the body undergoes significant physical and hormonal changes. Managing postpartum bleeding involves using menstrual pads and maintaining hygiene with peri rinse bottles or sitz baths. Pain relief can be supported with medications like ibuprofen or acetaminophen, ice packs, and heating pads.
Supporting recovery also includes wearing supportive postpartum underwear to assist pelvic floor healing and using stool softeners to ease constipation. Hemorrhoid creams for postpartum help manage discomfort common after childbirth. Breastfeeding supplies are essential, with items such as nursing pillows, nipple creams, and breast pumps aiding both comfort and milk production.
Emotional support networks and awareness of postpartum depression symptoms are vital as many new mothers face mood changes. Scheduling postpartum visits ensures ongoing health monitoring and access to mental health resources if needed.
What comprehensive obstetrical services are available in Queens, NY?
Queens offers extensive obstetrical and gynecological services through facilities like Women's Health at NYC Health + Hospitals/Queens, Women's Health at NewYork-Presbyterian Queens, and Long Island Jewish Forest Hills maternity care. These centers provide routine prenatal care, high-risk pregnancy management, labor and delivery services, and postpartum support. Advanced monitoring like ultrasonography and fetal heart monitoring is integral to their care.
Specialized programs support pregnant teenagers, women with gestational diabetes or infectious diseases, and families requiring NICU care for newborns. Multiple outpatient clinics offer flexible hours to ensure consistent access to care. Nutrition counseling, breastfeeding education, and mental health services complement medical treatment, promoting holistic maternal and infant health.
These comprehensive services ensure that women in Queens receive culturally sensitive, personalized, and continuous care throughout pregnancy and the postpartum period.
Comprehensive Pregnancy Care: A Path to Healthy Mothers and Babies
Integration of Nutrition, Exercise, and Monitoring
A balanced approach to pregnancy care in Queens, NY, emphasizes the integration of proper nutrition, safe exercise, and thorough fetal monitoring to support both mother and baby. Nutritional guidance encourages consuming essential nutrients like folic acid, iron, calcium, and omega-3 fatty acids, in line with increased caloric and fluid needs through pregnancy trimesters. Exercise, including moderate-intensity activities such as walking, swimming, and yoga, is safely encouraged to reduce the risks of gestational diabetes and promote smoother labor, while fetal monitoring ensures the baby's well-being by tracking heart rate and contractions to identify potential risks early on.
The Importance of Personalized Care and Local Healthcare Resources
Women benefit from personalized care tailored to their medical history and pregnancy risk factors. Healthcare providers in Queens offer comprehensive obstetric and gynecological services, including high-risk pregnancy management and postpartum support, through hospitals and clinics that provide culturally sensitive care, prenatal testing, ultrasound imaging, and access to specialized programs like WIC and tobacco cessation. Collaboration between patients and providers ensures individualized planning for delivery, nutrition, exercise, and monitoring, while considering personal preferences and health needs.
Encouragement for Women to Seek Support and Maintain Healthy Habits
Pregnancy is an ideal time for adopting healthy habits and accessing community support. Women are encouraged to maintain physical activity safely, follow nutritional recommendations, stay hydrated, and avoid harmful substances. Postpartum care includes managing recovery, breastfeeding, mental health monitoring, and regular follow-ups. Strong support networks, professional help, and education contribute to emotional well-being and physical health during and after pregnancy, promoting positive outcomes for mothers and babies alike.




.png)