Navigating VBAC: Key Insights for Expectant Mothers After Cesarean
Introduction to Laparoscopic Advances in Gynecology
Overview of Laparoscopic Surgery in Gynecology
Laparoscopic surgery, a form of minimally invasive surgery, uses a thin, lighted tube called a laparoscope inserted through small incisions to treat various gynecological conditions. Common procedures include hysterectomy, myomectomy, ovarian cystectomy, endometriosis treatment, and tubal ligation. This technique has become widely accepted due to its effectiveness and safety, replacing many traditional open surgeries.
Benefits of Minimally Invasive Procedures
Minimally invasive gynecologic surgeries offer significant advantages over conventional open surgery. These include smaller incisions, resulting in less scarring and reduced postoperative pain. Patients typically experience quicker recovery times, shorter hospital stays, and lower risks of infection and blood loss. These benefits translate to faster return to daily activities and improved overall patient satisfaction.
Importance of Technology in Modern Gynecological Care
Advancements in technology have played a crucial role in elevating laparoscopic procedures. Innovations like 3D and 4K imaging provide enhanced depth perception and anatomical detail, improving surgical precision. Robotic-assisted systems deliver greater dexterity and control, facilitating complex surgeries with better outcomes. These technological enhancements ensure safety, reduce complications, and support surgeon training, ultimately advancing patient care in gynecology.
Enhanced Visualization: The Shift from 2D to 3D and 4K Imaging

What are the Limitations of Traditional 2D Laparoscopy?
Traditional 2D laparoscopy, while minimally invasive, suffers from limited depth perception and reduced spatial orientation. These constraints demand higher surgeon skill to interpret flat images, increasing the challenge in complex gynecologic surgeries and potentially prolonging operative times.
How Does 3D Laparoscopy Improve Depth Perception and Spatial Orientation?
3D laparoscopy in gynecology significantly enhances 3D laparoscopy surgical performance by providing stereoscopic vision, which delivers true depth perception and better spatial awareness. This improvement leads to shorter operative times, less intraoperative blood loss, and quicker patient recovery, especially in delicate procedures like 3D laparoscopy for endometriosis and urogynecological 3D laparoscopy. Additionally, 3D systems facilitate training by shortening the 3D laparoscopy learning curve and improving surgical precision.
What Impact Does 4K Three-Dimensional Imaging Have on Surgical Precision?
The integration of ultra-high-definition Era of 4K three-dimensional imaging with 3D visualization offers up to four times the pixel density of standard HD, granting surgeons exceptional anatomical detail and clarity. This advanced imaging reduces surgical errors, enhances tissue differentiation, and improves safety during complex operations such as deeply infiltrating endometriosis removal and oncologic staging. The 4K 3D systems thus merge superior resolution with depth perception, bridging the gap between conventional laparoscopy and robotic technology.
How Does This Compare with Robotic Visualization Capabilities?
Robotic-assisted surgical systems, like the da Vinci platform, provide high-definition 3D vision combined with improved dexterity and tremor reduction. While robots offer advanced visualization similar to 3D laparoscopy, the latter is a cost-effectiveness of 3D laparoscopy alternative that achieves comparable outcomes without the high expenses and infrastructure demands of robotic systems. Technological advancements continue to enhance ergonomic challenges in 3D laparoscopy, potentially expanding its accessibility and adoption in gynecologic surgery.
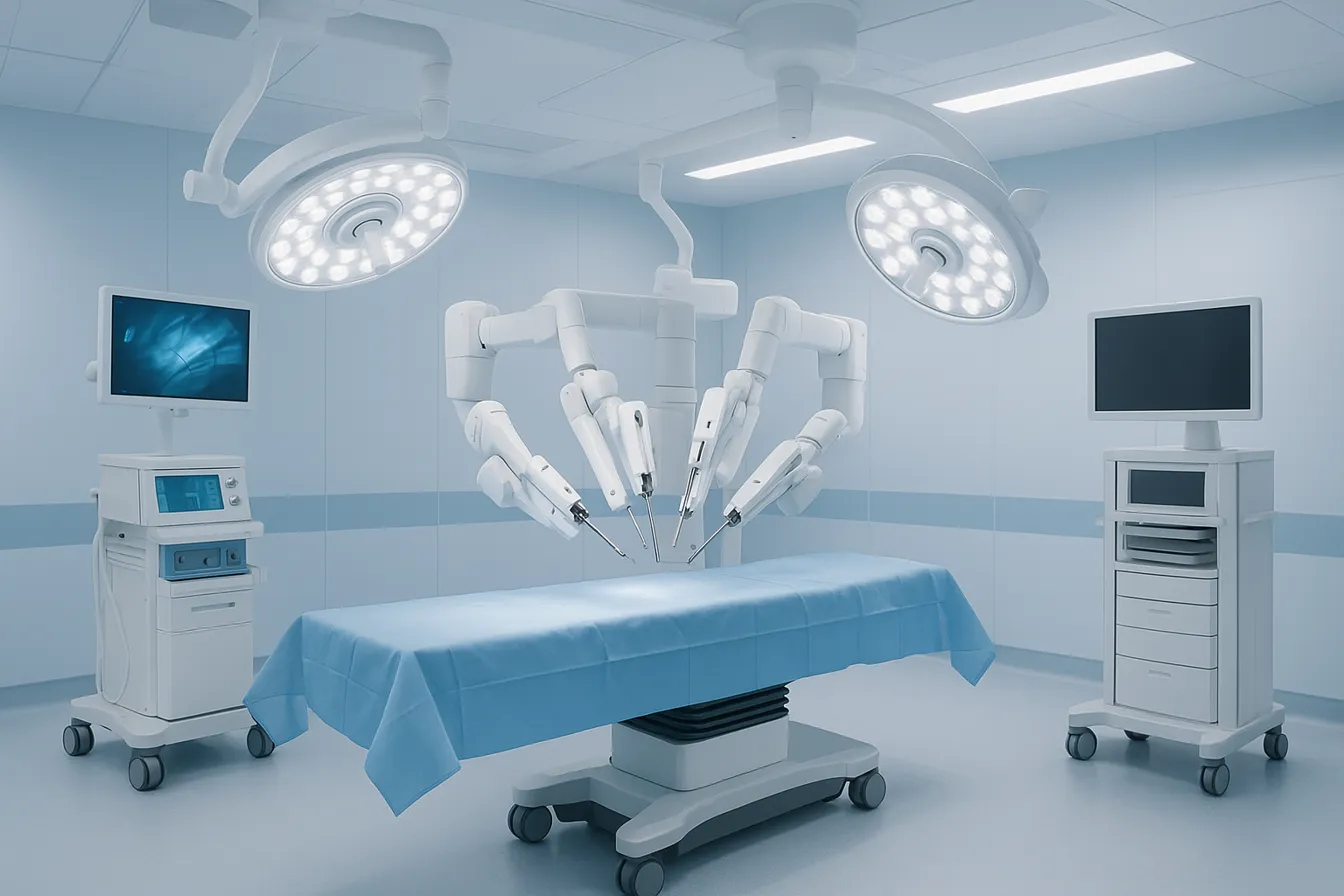
Robotic-Assisted Surgery: Precision and Ergonomics in Complex Gynecologic Procedures
How do robotic-assisted systems enhance precision and dexterity in gynecologic surgery?
Robotic-assisted surgery (RAS) utilizes advanced technology to provide surgeons with three-dimensional visualization, tremor cancellation, and articulated instruments that enhance precision and dexterity. Surgeons control robotic arms via a console, allowing for intricate maneuvers in confined pelvic spaces. This is particularly beneficial in complex gynecologic procedures such as hysterectomy, myomectomy, pelvic organ prolapse repair, and endometriosis treatment (Minimally invasive gynecologic surgery advances).
What are the benefits of robotic-assisted surgery in terms of patient outcomes?
Robotic-assisted surgery offers several advantages compared to traditional open or even conventional laparoscopic surgery. Benefits include:
- Smaller incisions that result in less postoperative pain and minimal scarring.
- Reduced blood loss during surgery due to improved surgical accuracy.
- Shorter hospital stays and quicker recovery times, facilitating faster return to daily activities.
- Enhanced ergonomic comfort for surgeons, which can reduce fatigue and improve surgical focus (Robotic-assisted surgical systems, Advantages of robotic gynecologic surgery.
How is artificial intelligence (AI) integrated into robotic surgery and what future trends are expected?
The integration of AI in robotic gynecologic surgery is an emerging field aiming to optimize surgical outcomes. AI enables:
- Real-time intraoperative decision support, allowing tailored treatment strategies.
- Enhanced imaging analysis for better surgical planning. Future technological trends include autonomous surgical functions, improved imaging modalities, expanded use of single-port robotic systems such as vaginal natural orifice transluminal endoscopic surgery (vNOTES), and remote robotic surgery to increase access in underserved regions (Future of robot-assisted surgery in gynecology).
What challenges limit the widespread adoption of robotic-assisted gynecologic surgery?
Despite its advantages, robotic surgery faces several barriers:
- High costs of acquisition and maintenance limit availability primarily to high-volume medical centers.
- The steep learning curve demands structured and prolonged surgeon training.
- Risks related to equipment malfunctions and procedural safety.
- Ethical concerns, including data privacy and implications of remote surgery.
- Need for continued research to prove cost-effectiveness in broader healthcare settings (Robotic surgery challenges.
Robotic-assisted surgery represents a transformative advancement in gynecologic care, balancing surgical precision and patient safety. Ongoing innovations and expanded surgeon training will likely overcome current obstacles to make this technology more accessible to a broader patient population (Minimally invasive gynecologic surgery.
Innovations in Surgical Techniques and Instruments

What are the emerging minimally invasive approaches in gynecologic surgery?
Emerging techniques such as single-incision laparoscopic surgery (SILS) and transvaginal natural orifice transluminal endoscopic surgery (vNOTES) are advancing the field of minimally invasive gynecologic surgery. Both approaches prioritize reducing surgical invasiveness and scarring. SILS uses a single small incision, often at the navel, which enhances cosmesis and may reduce postoperative pain. vNOTES accesses pelvic organs via the vagina without abdominal incisions, offering the benefit of scarless procedures with faster recovery and less pain.
How have laparoscopic entry methods and morcellation techniques improved?
Laparoscopic entry techniques including the Veress needle, open (Hasson), and direct trocar methods all demonstrate comparable safety when applied by experienced surgeons. Current evidence recommends surgeons use the method they are most familiar with for optimal safety. Regarding tissue extraction, morcellation has evolved to prioritize safety following FDA warnings about tissue dissemination risks, especially occult sarcoma spread. Containment systems and in-bag morcellation are now widely adopted to reduce these risks.
What is the significance of barbed sutures in laparoscopic procedures?
Barbed sutures, such as V-Loc, have revolutionized laparoscopic surgeries like hysterectomy and myomectomy. These sutures distribute tension evenly along the suture line and eliminate the need for knot tying, which significantly reduces operative time and lowers complication rates. Their use facilitates efficient tissue closure, enhances surgical safety, and supports quicker recovery.
How do enhanced recovery after surgery (ERAS) protocols benefit patients?
ERAS protocols optimize perioperative care through coordinated pre-, intra-, and postoperative measures. In gynecologic minimally invasive surgery, ERAS has been shown to decrease hospital stays, reduce opioid use, lower costs, and improve overall patient satisfaction. These protocols contribute to faster recovery and better clinical outcomes by promoting early mobilization, effective pain management, and nutritional support.
In sum, these innovations in surgical techniques and instruments continually improve the safety, efficiency, and patient experience in minimally invasive gynecologic surgery.
Preoperative Imaging and Surgical Planning Enhancements

How is advanced ultrasound used in gynecologic surgery?
Advanced ultrasound techniques, including three-dimensional (3D) imaging and standardized protocols like the International Deep Endometriosis Analysis (IDEA), play a crucial role in accurately diagnosing endometriosis. These modalities improve visualization of lesions such as endometriomas and deep infiltrative endometriosis, offering high sensitivity (up to 94%) and specificity (up to 97%). Enhanced ultrasound reduces the need for surgical diagnosis by providing detailed preoperative assessments that guide surgical planning. For more detailed information, see benign gynecological laparoscopic advances, preoperative imaging in gynecology, ultrasound and MRI for gynecological surgery planning, ultrasound protocols for endometriosis diagnosis, 3D ultrasound and rectal water contrast, MRI assessment of endometriosis and fibroids, laparoscopic entry techniques.
What is the role of MRI in surgical planning for complex gynecologic cases?
Magnetic resonance imaging (MRI) serves as a vital second-line imaging tool, especially when ultrasound findings are inconclusive or in cases involving multiple fibroids or adenomyosis. MRI offers detailed characterization and staging of pelvic pathologies, enabling precise mapping of fibroid size, number, and location. This detailed imaging helps surgeons devise personalized approaches that improve surgical outcomes, particularly in complex cases requiring extensive excision or fertility preservation. More about minimally invasive gynecologic surgery and preoperative imaging for endometriosis can be explored.
How do imaging advancements contribute to personalized surgical planning and outcomes?
By combining high-resolution ultrasound and MRI, clinicians can tailor surgical strategies to individual patient anatomy and pathology. These imaging advances facilitate accurate lesion localization, reduce operative times, and minimize intraoperative blood loss. They also enable fertility-sparing procedures and optimal management of conditions like endometriosis and fibroids, resulting in quicker recovery periods, less postoperative pain, and higher patient satisfaction. Learn more about minimally invasive gynecologic surgery, benefits of minimally invasive surgery, laparoscopic surgery, and personalized care in gynecologic surgery.
What is the impact of multidisciplinary approaches enabled by imaging advances?
The integration of advanced imaging fosters collaboration among gynecologists, radiologists, and surgeons, supporting multidisciplinary case discussions. This teamwork allows comprehensive planning and management of complex gynecologic disorders. It enhances diagnostic accuracy, guides minimally invasive surgical techniques, and supports decision-making regarding the safest and most effective interventions, ultimately advancing patient-centered care in gynecology. For insight into Cedars-Sinai gynecologic surgery advances and minimally invasive gynecologic surgery research visit the resource.
Training and Cost-Effectiveness: Broadening Access to Advanced Laparoscopic Care
How does 3D laparoscopy enhance surgical training and shorten learning curves?
3D laparoscopy significantly improves spatial awareness and depth perception for surgeons, which facilitates skill acquisition. Research shows that especially for 3D laparoscopy for trainee surgeons, 3D visualization helps shorten the traditionally steep 3D laparoscopy learning curve inherent in minimally invasive 3D laparoscopy in gynecology. This results in enhanced 3D laparoscopy surgical performance and confidence early in their training.
What role does simulation-based training play in surgeon proficiency and patient safety?
Simulation-based training, utilizing virtual reality and hybrid models, provides a safe environment for surgeons to develop and refine laparoscopic skills before operating on patients. Such training enables objective assessment and credentialing, thus enhancing patient safety by ensuring surgeons are well-prepared for complex procedures.
How does 3D laparoscopy compare to robotic systems in terms of cost-effectiveness?
3D laparoscopy offers a cost-effectiveness of 3D laparoscopy alternative to Robotic-assisted surgical systems by providing comparable clinical outcomes, including improved precision and reduced operative times. It requires less expensive equipment and infrastructure, making it particularly valuable in resource-limited settings, where high robotic system costs may limit accessibility.
What barriers remain for the widespread adoption of 3D laparoscopy?
Despite technological advances that have improved ergonomics in 3D laparoscopy and reduced some surgeon fatigue, issues such as eye strain in 3D laparoscopy still exist. Additionally, high initial costs for equipment, as well as the need for specialized training and institutional resources, pose challenges to broader implementation in many healthcare settings.
Together, these factors underscore the importance of integrating advanced training methods and cost-friendly technologies like 3D laparoscopy to expand access to minimally invasive gynecologic surgery while maintaining high standards of patient care.
Future Outlook: Integrating Technology to Enhance Patient-Centered Gynecologic Care
Advancing Minimally Invasive Gynecology
Minimally invasive gynecologic surgery is continuously evolving with innovations in 3D and robotic technologies enhancing surgical precision and recovery times. These advancements improve patient outcomes by reducing pain, blood loss, and hospital stays.
Emerging Role of Artificial Intelligence and Remote Surgery
The integration of artificial intelligence offers real-time decision support and personalized surgical strategies. Remote robotic surgery holds promise for increasing access to specialized care in underserved areas, potentially transforming gynecologic treatment delivery.
Emphasizing Personalized Care
Technological advancements support tailored treatments that address individual patient needs, enhancing satisfaction and recovery. Surgeons leverage enhanced visualization and data-driven insights to optimize outcomes.
Outlook for Wider Adoption
As these technologies mature and become more cost-effective, broader adoption in diverse healthcare settings is anticipated, expanding access and maintaining high standards of care globally.




.png)