Bridging Traditions and Innovations to Transform Pregnancy Care
Understanding the Synergy in Pregnancy Care
Overview of the evolving landscape of pregnancy care
Pregnancy care has undergone significant transformation, blending long-standing traditional practices with modern evidence-based methodologies. This fusion ensures comprehensive support for both mother and child, reflecting a commitment to safety, effectiveness, and cultural sensitivity throughout prenatal, birth, and postpartum stages.
Importance of combining traditional and modern methods
Historically, diverse cultural approaches—such as herbal remedies, massage, breathing techniques, and specific postpartum rituals—have played vital roles in maternal health. Modern pregnancy care embraces these while incorporating scientific advancements, such as precise medical screenings, personalized risk assessments, and innovative monitoring technologies. This dual approach respects heritage and adapts to contemporary healthcare standards, enhancing overall care quality.
Benefits of integrating diverse care strategies for maternal and infant health
Integrating traditional wisdom with modern care leads to holistic health benefits, including improved physical, emotional, and spiritual well-being. Personalized care plans and continuous support contribute to better birth outcomes, greater maternal confidence, and stronger mother-infant bonding. Collaborative care involving midwives, obstetricians, and other specialists ensures tailored interventions, addressing unique needs and social determinants that impact health equity. This synergy fosters a more empowered and healthier pregnancy journey for families.
Holistic Approaches to Maternity Care: Embracing the Whole Woman
What is the holistic approach to maternity care?
Holistic approaches to pregnancy look beyond just the physical health of a pregnant woman to encompass emotional, mental, social, and spiritual well-being throughout pregnancy, childbirth, and postpartum. This method respects and supports the natural processes of conception, nourishment, and birth while tailoring care to each woman's unique values, beliefs, and cultural practices.
Physical, emotional, mental, social, and spiritual aspects in care
Holistic approach to midwifery addresses physical health through proper nutrition, regular prenatal checkups, and management of common pregnancy discomforts. It also prioritizes emotional and mental well-being by integrating stress reduction techniques and ensuring strong social support networks, including family and doulas. Spiritual care, often overlooked in conventional models, is honored by respecting cultural customs and offering compassionate, continuous support during labor and recovery.
Complementary therapies such as acupuncture, massage, and mindfulness
Complementing modern medicine, holistic maternity care incorporates therapies like massage therapy in midwifery, acupuncture to manage nausea and pain, and prenatal yoga and mindfulness or prenatal yoga to improve mental clarity and reduce anxiety. These evidence-based complementary methods help minimize unnecessary medical interventions and promote natural labor progression.
Empowerment through informed decision-making and natural labor support
Central to this approach is empowering women by providing comprehensive education empowerment for women on pregnancy, childbirth, and postpartum care. Women are encouraged to participate actively in decision-making, create personalized birth plans, and rely on natural pain management techniques such as breathing techniques during labor, visualization, and movement. This empowerment fosters confidence, reduces fear, and helps women experience birth on their terms with respectful support from caregivers.
Overall, embracing holistic maternity care means nurturing the whole woman with compassionate, personalized, and evidence-informed support to promote healthier pregnancies and more satisfying birth experiences.
Traditional Prenatal Care: The Foundation of Maternal Health
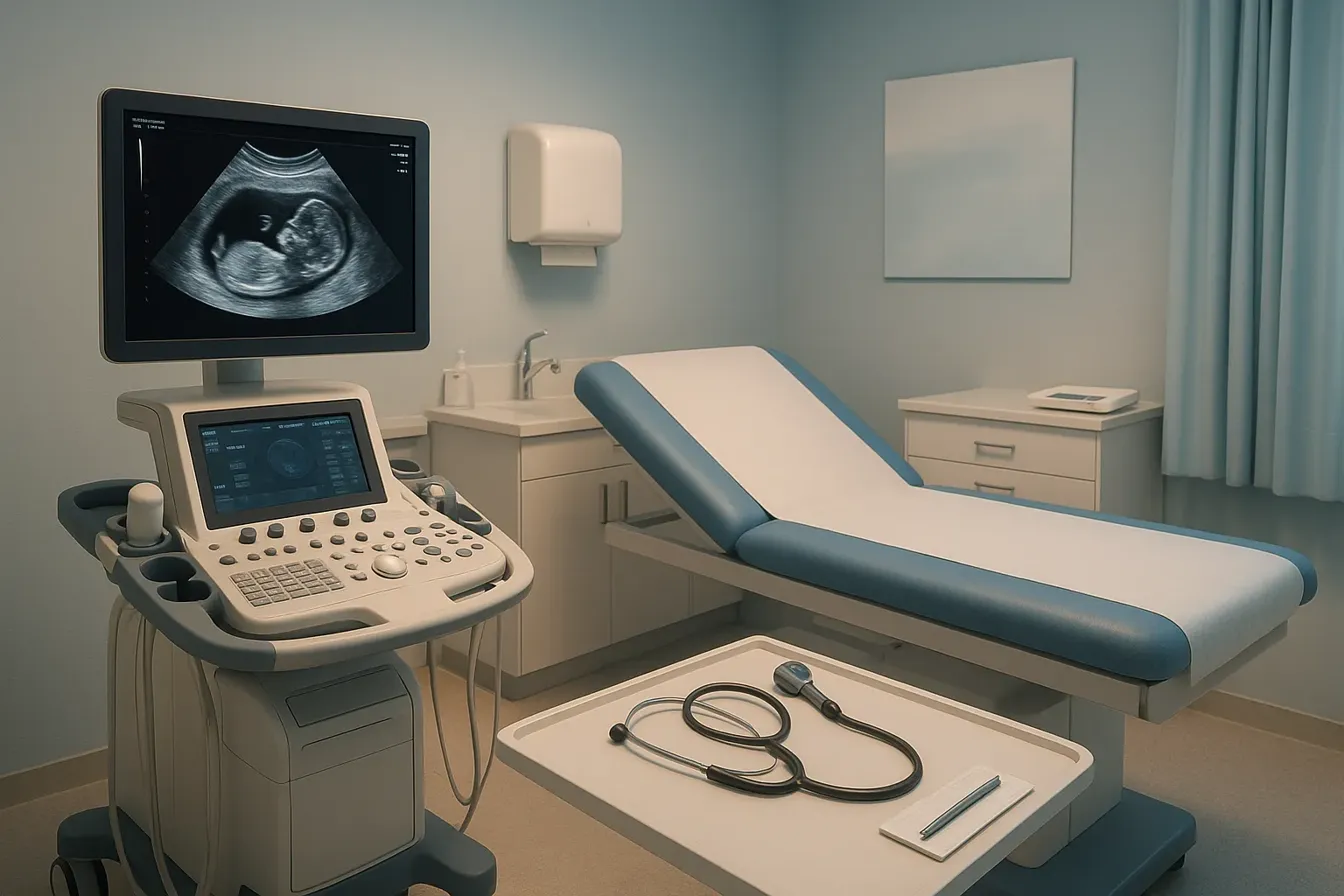
What is traditional prenatal care?
Traditional prenatal care is a comprehensive approach that begins once pregnancy is suspected or confirmed. It involves regular visits to healthcare providers where Tailored Prenatal Care Delivery are closely monitored through physical exams, weight checks, urine and blood tests, and ultrasound scans. This ongoing care supports both mother and baby throughout the different stages of pregnancy.
Routine prenatal visits and screenings
During these visits, routine screenings assess the mother's health and the baby's development. Blood pressure monitoring, fetal heart tones, and fundal height measurements help detect any abnormalities early. Blood tests screen for anemia, infections, and other conditions, while ultrasounds provide visual assessments of fetal growth.
Monitoring maternal and fetal health
Continuous monitoring is crucial to identify potential risks such as gestational diabetes, preeclampsia, or fetal growth restrictions. Early detection through prenatal care allows timely intervention, improving outcomes for mother and infant.
Nutritional guidance and vaccination
Prenatal care includes nutritional counseling to promote adequate weight gain and necessary vitamin intake, such as folic acid, which reduces neural tube defects. Pregnant women are advised to avoid harmful substances like alcohol, tobacco, and certain raw foods. Vaccinations like the influenza shot and Tdap are recommended to protect both mother and baby from severe infections.
Importance of early and consistent care
Starting prenatal care within the first trimester is critical, as it significantly decreases risks of low birth weight and infant mortality. Consistency in care ensures ongoing health assessments and timely management of any complications.
Preconception health preparation
Traditional prenatal care extends to pre-pregnancy planning, encouraging women to prepare their bodies through proper nutrition, cessation of harmful habits, and management of chronic conditions. This foundation sets the stage for a healthy pregnancy journey.
| Aspect | Purpose | Benefits |
|---|---|---|
| Routine screenings | Assess maternal and fetal health | Early detection of risks, better outcomes |
| Nutritional guidance | Support healthy weight gain and fetal development | Reduce birth defects and complications |
| Vaccinations | Prevent maternal and neonatal infections | Safer pregnancy and newborn health |
| Early and regular visits | Comprehensive and timely care | Lower risks of poor birth outcomes |
| Preconception care | Optimize health before pregnancy | Improved pregnancy and delivery results |
The 5 P's of Pregnancy: Key Factors in Labor and Childbirth
What are the 5 P's of pregnancy and why are they important?
The 5 P's of pregnancy—Power, Passageway, Passenger, Positioning, and Psyche—are fundamental elements that play a crucial role in labor and childbirth outcomes.
- Power refers to the strength, frequency, and effectiveness of uterine contractions that drive the baby through the birth canal. Adequate power is essential for labor to progress efficiently.
- Passageway encompasses the mother's birth canal, including the bony pelvis and soft tissues. The size and shape of this passageway greatly influence the ease with which the baby can be delivered.
- Passenger relates to the fetus itself, focusing on its size, presentation (such as head-first or breech), and position within the uterus. These aspects impact how smoothly delivery occurs.
- Positioning involves the orientation and posture of the baby during labor, including movements and rotations needed to navigate the birth canal.
- Psyche addresses the mother's mental and emotional state. Stress, anxiety, and fear can affect the body's natural ability to progress labor and influence pain perception.
Impact on labor progress and delivery outcomes
Each of these factors interacts to influence the duration and experience of labor. For example, strong and well-timed uterine contractions (Power) combined with optimal fetal positioning (Positioning support a smoother delivery. Conversely, an unfavorable pelvis shape (Passageway or fetal malpresentation (Passenger can complicate childbirth, potentially indicating the need for specialist intervention.
Emotional well-being (Psyche also directly affects labor hormones and pain management, highlighting the importance of compassionate support and stress reduction techniques during labor.
How understanding the 5 P's improves personalized care and management
By closely monitoring and assessing each of the 5 P's, healthcare providers can tailor care plans to the individual needs of the mother and baby. This might involve techniques like repositioning the mother to enhance fetal descent, offering relaxation strategies to ease stress, or preparing for medical interventions when passageway or passenger issues arise.
This comprehensive understanding promotes safer labor, optimizes outcomes, and enhances maternal satisfaction by respecting each mother's unique physical and emotional context. Incorporating knowledge of the 5 P's aligns with modern midwifery, blending tradition with evidence-based care, empowering women and supporting positive childbirth experiences.
Modern Trends to Personalize Childbirth Experiences
What are some modern trends to personalize childbirth?
Modern childbirth is witnessing a profound shift towards personalization and holistic care, integrating diverse natural and traditional practices alongside medical advances to enrich the birthing experience. Many parents seek to embrace supportive, calming methods such as hypnobirthing—using guided relaxation and focused breathing to reduce anxiety and pain during labor. Water births have also gained popularity, offering a gentle transition for the newborn and a soothing environment for laboring mothers.
Acupuncture is another complementary technique employed to naturally manage pain and facilitate labor progression. These holistic options emphasize minimizing unnecessary medical interventions, promoting a natural birthing process where women feel empowered and in control.
The creation of personalized birth plans is central to this approach, allowing expectant mothers to communicate their preferences clearly with healthcare providers. Such plans integrate both natural practices and evidence-based care, fostering autonomy and confidence throughout labor and delivery.
Collectively, these trends reflect a broader commitment in maternity care to blend tradition, innovation, and personalized support, enhancing physical comfort and emotional well-being for both mother and baby.
The Role and Advantages of Traditional Birth Attendants
What are the advantages of traditional birth attendants?
Traditional birth attendants (TBAs) provide personalized and culturally sensitive care, honoring local childbirth customs and practices. This approach fosters trust and comfort for mothers, who often feel more supported and understood when their cultural norms are respected.
TBAs are particularly vital in remote or underserved communities where access to formal healthcare facilities may be limited or non-existent. They enhance maternal care accessibility by being more readily available and often more affordable than hospital-based care.
During labor and delivery, TBAs offer continuous emotional and physical support. Their presence provides reassurance and advocacy for women, which has been shown to reduce stress and improve birth experiences.
However, TBAs may face limitations as they often lack the capability to manage complications or high-risk pregnancies requiring advanced medical intervention. Therefore, integrating TBAs with the formal medical care system ensures that women can benefit from both culturally sensitive support and timely medical care when necessary.
Combining the ancestral knowledge and personalized care of TBAs with the resources and expertise of modern medical facilities creates a comprehensive maternal health support system, improving outcomes for both mothers and infants.
Integrating Traditional and Modern Healthcare: Enhancing Pregnancy Care
What Are the Benefits of Combining Traditional and Modern Healthcare Methods?
Integrating traditional healthcare methods, like herbal remedies in midwifery and acupuncture, with evidence-based modern medicine offers a comprehensive maternal and infant care approach for pregnant individuals. Traditional practices contribute holistic approaches to pregnancy, addressing physical, emotional, and spiritual needs, often with fewer side effects. For example, massage therapy in midwifery and herbal therapies have been used effectively in various cultures to support pregnancy wellness.
Modern medicine provides scientific precision in diagnosing and treating pregnancy-related complications, ensuring safety and effectiveness through rigorous research. When combined, these approaches allow healthcare providers to craft personalized midwifery care plans respectful of cultural backgrounds while grounded in clinical evidence.
Tailoring Treatments to Patients' Cultural Backgrounds
Recognizing and incorporating patients' cultural beliefs and traditional beliefs in pregnancy enhances trust and engagement in prenatal and postpartum care. For instance, many Asian communities practice postpartum confinement traditions and use specific herbal remedies to promote recovery. Integrating such customs within modern care models supports maternal well-being and community values.
Healthcare providers skilled in cultural sensitivity and collaborative care can bridge gaps by respecting ancestral knowledge and providing education on safe practices. This Tailored Prenatal Care Delivery approach contributes to higher satisfaction and better health outcomes.
Benefits of Integration for Safety, Effectiveness, and Patient Satisfaction
This fusion promotes enhanced modern midwifery, blending tradition with evidence-based care. It nurtures emotional support, reduces stress, and encourages natural bonding techniques like skin-to-skin contact benefits.
Moreover, integrating traditional wisdom in midwifery with modern techniques minimizes risks and improves treatment adherence. Patients feel empowered through informed decision-making, receiving continuous support adapted to their unique needs.
Overall, this holistic midwifery approach leads to safer pregnancies, more positive birth experiences, and long-term health benefits for families.
Group Prenatal Care: Fostering Community and Improving Outcomes
What are the benefits of group prenatal care?
Group prenatal care models, such as CenteringPregnancy model and Enhanced Antenatal Care (EAC), provide pregnant women with extended time for health assessments, education, and peer support in a group setting. Unlike the traditional model with brief individual visits, classes typically last 90 minutes to two hours and integrate individualized health checks with interactive discussions on pregnancy, labor, postpartum care, and newborn parenting.
Benefits of group prenatal care include:
- Reduced Preterm Births and Low Birth Weight: Studies show decreased rates of preterm birth and improved birth weights, particularly among low-income and minority populations.
- Improved Breastfeeding Initiation and Duration: Women in group care are more likely to start and continue breastfeeding successfully.
- Increased Prenatal Knowledge and Preparedness: Education during sessions covers vital topics, empowering women with knowledge about nutrition, stress management, labor, and postpartum health.
- Enhanced Maternal Satisfaction and Engagement: Women report feeling better prepared for labor and delivery and more satisfied with their care experience.
- Social Support and Peer Encouragement: Group settings foster connection and emotional support among pregnant women, improving mental well-being and adherence to prenatal visits.
How does group prenatal care foster social support?
The group prenatal care model encourages peer-to-peer interaction, creating a community where participants share experiences, concerns, and advice. This social bonding reduces isolation, nurtures confidence, and provides a platform for mutual encouragement. The presence of supportive peers can lessen fear of childbirth and enhance coping strategies, contributing to a healthier pregnancy journey.
What challenges exist in implementing and sustaining group prenatal care?
Despite the evident benefits, widespread adoption faces hurdles including:
- Organizational Demands: Successful programs require dedicated space, leadership support, and committed staff.
- Funding and Reimbursement: Sustainable financing and insurance reimbursement policies are needed to maintain operations.
- Provider Buy-in: Some healthcare providers may be hesitant to relinquish traditional control over prenatal visits, fearing loss of individual patient attention.
- Leadership Changes: Shifts in organizational priorities can disrupt continuity of group care.
Effective implementation relies on integration into routine practice, collaboration between staff, and systemic support for reimbursement.
In summary, group prenatal care offers a holistic, patient-centered approach that combines clinical assessment with education and social support to improve both physical and emotional pregnancy outcomes. Its expansion promises to reduce disparities and foster healthier communities.
Tailored Prenatal Care: Adapting to Individual Needs and Challenges
Importance of Early Risk Assessment and Individualized Plans
Early and thorough risk assessments during pregnancy are essential for optimal health outcomes. Ideally conducted before 10 weeks of gestation, these assessments evaluate medical, social, and structural factors influencing maternal and fetal well-being. Individualized care plans developed collaboratively with pregnant individuals empower them and tailor healthcare interventions to their unique needs. This approach improves satisfaction and mitigates adverse outcomes by creating flexible, patient-centered strategies that evolve throughout pregnancy. For detailed insights, see Tailored Prenatal Care Delivery.
Addressing Social Determinants of Health
Social determinants such as race, socioeconomic status, geography, and access to resources significantly affect prenatal care quality and timing. Tailored prenatal care focuses on identifying these social barriers early, offering referrals to assistance programs and community resources. Addressing issues like transportation, housing instability, food insecurity, and systemic bias helps bridge gaps in care, particularly for marginalized populations, decreasing health disparities and improving maternal and neonatal outcomes. For more information, refer to Tailored Prenatal Care Delivery.
Use of Telemedicine and Flexible Scheduling
Innovative prenatal care models incorporate telemedicine and alternative visit schedules to enhance access and convenience. Virtual consultations, remote monitoring, and group prenatal care settings increase engagement and reduce logistical burdens for expectant mothers, especially those facing transportation challenges or work constraints. This flexible scheduling fosters ongoing communication with healthcare teams, allows shared decision-making, and ensures timely interventions without unnecessary in-person visits. Learn more about these advancements at Digital transformation of maternity care and Tailored Prenatal Care Delivery.
Self-Monitoring Innovations for Maternal Health Parameters
Modern prenatal care increasingly supports self-monitoring by patients as a feasible and effective strategy. Pregnant individuals are trained to track key health parameters such as blood pressure, weight, and fetal heart tones at home, using user-friendly devices. Emerging wearable technologies including smartwatch-like wristbands, abdominal sensors, sensor belts, electrode patches, and soft electronic devices enhance remote monitoring capabilities. These tools facilitate early detection of complications and promote active participation in care, improving maternal and fetal health outcomes. More details are available in Tailored Prenatal Care Delivery.
| Aspect | Description | Benefits |
|---|---|---|
| Early Risk Assessment | Evaluation before 10 weeks, individualized plans | Improves outcomes, fosters shared decision-making |
| Social Determinants Addressed | Referrals and assistance for unmet social needs | Reduces disparities, supports vulnerable groups |
| Telemedicine & Flexible Visits | Remote consultations, alternative scheduling | Enhances access, reduces barriers |
| Self-Monitoring Technologies | Devices for blood pressure, weight, fetal heart | Empowers patients, enables timely detection |
Addressing Disparities in Prenatal Care and Maternal Outcomes in the US
What Racial, Socioeconomic, and Geographic Disparities Affect Prenatal Care in the US?
Significant disparities exist in the accessibility and quality of prenatal care across the United States, heavily influenced by race, socioeconomic status, and geographic location. Black, Hispanic, and American Indian/Alaska Native women are less likely to initiate prenatal care early and receive comprehensive services compared to their white counterparts. Rural areas are disproportionately affected by shortages of obstetric providers and maternity units, resulting in “maternity care deserts” covering about 36% of U.S. counties. These inequalities contribute to worse maternal and neonatal outcomes, including higher rates of preterm birth and low birth weight. Maternal and Newborn Care in the United States
What Are the Barriers to Early Prenatal Care and High-Quality Services?
Barriers include lack of insurance coverage or underinsurance, systemic discrimination and implicit bias within healthcare, transportation challenges, and limited availability of culturally sensitive care. Social determinants of health such as poverty, food insecurity, and unstable housing also impede timely access to prenatal visits and recommended screenings. Nearly one-quarter of pregnant individuals delay establishing prenatal care until after the first trimester, and almost half do not receive all essential services promptly. Tailored Prenatal Care Delivery
What Initiatives Aim to Improve Access and Equity?
Efforts to reduce these disparities include Medicaid expansion, which covers about 43% of all births and plays a critical role for high-risk populations. Home visiting programs and community health worker engagement provide additional support for at-risk mothers. Implicit bias training for healthcare professionals and improved cultural competence promote respectful, patient-centered care. Telehealth services and group prenatal care models, like Group prenatal care benefits, enhance accessibility and provide supportive environments especially for marginalized groups.
How Do Diverse Care Providers Like Midwives and Doulas Support Better Outcomes?
Certified nurse-midwives, family physicians, and doulas are integral to expanding maternity care access, particularly in underserved areas. Modern midwifery care combines evidence-based medical practice with personalized, holistic support, emphasizing empowerment and education. Doulas provide continuous emotional and physical support throughout pregnancy and childbirth, which has been shown to improve maternal satisfaction and decrease intervention rates. Partnerships among these providers enhance comprehensive care and address complex social and medical needs.
Where Does the US Rank in Maternal Care Compared to Other Developed Countries?
Despite its technological advancements and resources, the United States faces a maternal mortality rate of 32.9 deaths per 100,000 live births as of 2021—ranking it 55th globally and among the worst in developed nations. Maternal mortality rates have worsened in recent years, with approximately 80% of maternal deaths considered preventable. Black women experience nearly triple the risk of maternal death compared to white women, underscoring the urgent need to address systemic inequities and ensure equitable, accessible maternity care for all women. Maternity Care in the United States
The Evolving Role of Midwifery: Tradition Meets Evidence-Based Practice
Historical evolution of midwifery
Midwifery has a rich history marked by the integration of ancient midwifery practices with contemporary scientific research in midwifery. Traditionally rooted in community knowledge, midwifery today combines evidence-based maternal health care with time-honored practices to provide comprehensive maternal and infant care. This blend ensures that women receive support that respects cultural heritage while upholding safety and effectiveness.
Integration of traditional herbal remedies, massage, and breathing techniques
Modern midwifery incorporates natural methods such as herbal remedies in midwifery including chamomile, massage therapy for childbirth, specialized breathing techniques in labor, and optimal positioning strategies during childbirth. These practices, once passed down through generations, are now validated and refined through scientific study to enhance maternal comfort, reduce stress, and improve labor outcomes.
Personalized, continuous care and maternal empowerment
A hallmark of contemporary midwifery is the development of personalized midwifery care plans tailored to each woman’s unique physical, emotional, and cultural needs. Midwives prioritize continuous childbirth support from pregnancy through postpartum, emphasizing empowering women through education. By providing evidence-based maternal health care information and fostering informed decision-making, midwives enable women to actively participate in their care, leading to greater confidence and improving maternal and infant outcomes.
Collaborative care models involving obstetricians and specialists
Midwifery care often functions within multidisciplinary collaborative care teams that include obstetricians, pediatricians, lactation consultants, and mental health professionals. This collaboration ensures that both routine and complex cases receive maternal and infant health monitoring and intervention when needed. By bridging traditional and medical expertise, these models enhance safety and satisfaction for mothers and infants alike.
Cultural Traditions and Postpartum Care: The Role of Confinement and Support

What are traditional postpartum practices such as confinement periods?
Traditional postpartum care often involves a confinement period, a culturally significant time typically lasting 30 to 40 days, during which new mothers rest and focus on recovery. This practice is common in many Asian cultures, including Chinese communities where it is known as the "postpartum confinement traditions" period. Women are considered physically fragile and vulnerable to illness, so strict rest and specific rituals like dietary regulations, massage, and herbal remedies are emphasized to promote healing.
Why are rest, nutrition, and emotional support important postpartum?
Rest is critical during the postpartum period to help the body heal after childbirth. Nutritional guidance, often incorporating traditional herbs and balanced diets, supports tissue repair and replenishes energy. Emotional support fosters a mother's mental well-being, reduces stress, and promotes bonding with the infant. Holistic postpartum care addresses physical, emotional, and spiritual needs, which can improve long-term maternal health. For more on the Holistic postpartum health approach, see the linked resource.
How are traditional postpartum practices integrated with modern postpartum care services?
Modern postpartum care increasingly embraces traditional practices by blending them with evidence-based medical support. Healthcare providers recognize the benefits of nutritional guidance, massage, and rest while ensuring close monitoring of maternal recovery and infant health. Collaboration among midwives, obstetricians, lactation consultants, and mental health professionals helps create personalized midwifery care plans that respect cultural values while addressing clinical needs.
What roles do partners play and what gaps exist in postpartum wellness evaluation?
Partners are vital support figures during postpartum but often lack dedicated wellness checks or mental health screenings. This gap in care acknowledges a need for more inclusive postpartum services that involve partners to promote family well-being. Enhancing partner support and integrating their health evaluations can strengthen postpartum recovery environments and reduce stress for mothers.
Traditional postpartum care, especially the emphasis on confinement and support systems, remains an essential foundation that modern care models strive to respect and incorporate, advancing holistic health and well-being for mothers and families. For detailed discussions on Traditional beliefs in pregnancy and Traditional postpartum care practices in Mardin, see the linked resources.
Prenatal Nutrition and Lifestyle: Time-Tested and Modern Guidelines
Nutritional Recommendations Including Folic Acid Intake
Proper nutrition is fundamental for a healthy pregnancy. Experts recommend daily folic acid supplementation of 400 to 800 micrograms, starting at least one month before conception. This important vitamin reduces the risks of neural tube defects in the developing fetus. Prenatal care programs emphasize balanced nutrition, including adequate intake of iron, calcium, and protein, to support the mother’s increased physiological needs (Prenatal care overview).
Avoidance of Harmful Substances
Pregnant individuals are advised to avoid substances that could harm the baby, including smoking, alcohol, and certain foods. Fish with high mercury levels, raw or undercooked meats, and sources of toxoplasmosis such as cat feces should be avoided. These precautions reduce risks of developmental complications and infections (Prenatal care overview.
Importance of Weight Management and Physical Activity
Maintaining an appropriate weight gain during pregnancy is crucial. Healthcare providers monitor weight and encourage healthy dietary choices to prevent excessive or insufficient weight gain, both of which carry risks. Likewise, moderate physical activity tailored to the individual’s health status, including prenatal yoga, is encouraged. Exercise supports cardiovascular health, reduces stress, and may ease certain pregnancy symptoms (Holistic approaches to pregnancy).
Vaccinations During Pregnancy
Vaccinations like the influenza vaccine and the Tdap vaccine (given between 27 and 36 weeks of gestation) are recommended. These vaccines protect both the mother and newborn from serious infections, especially pertussis (whooping cough) and influenza, which can be severe during pregnancy (Family-centered prenatal care).
Benefits of Prenatal Yoga and Mindfulness
Integrating prenatal yoga and mindfulness practices during pregnancy promotes both physical flexibility and mental well-being. These holistic approaches reduce stress levels and enhance relaxation, helping expectant mothers prepare for childbirth. Mindfulness techniques also empower women by improving emotional resilience and enhancing the overall pregnancy experience (Holistic approaches to pregnancy.
These guidelines combine traditional knowledge and evidence-based care to ensure a safe and positive pregnancy journey, supporting maternal and infant health outcomes (Modern midwifery.
Innovative Technologies and Digital Health in Pregnancy Care

What are some new technologies used to monitor pregnancy remotely?
Remote pregnancy monitoring has evolved with the development of wearable technologies designed to track maternal and fetal health from a distance. Devices such as smartwatch-like wristbands, abdominal sensors, sensor belts, bodysuits, electrode patches, and soft electronic devices enable real-time collection of vital data without requiring frequent in-person visits. These tools allow pregnant individuals to monitor parameters like fetal heart rate, maternal blood pressure, and activity levels in the comfort of their homes, empowering them to actively engage in their prenatal care. Such innovations are part of the broader Femtech revolution in pregnancy care and the Digital transformation of maternity care.
Telemedicine and Hybrid E-Health Perinatal Clinics
Hybrid e-health perinatal clinics leverage telemedicine to provide comprehensive care by combining virtual consultations with in-person visits when necessary. This model addresses barriers to access, especially for those living in underserved or remote areas, by facilitating continuous monitoring and timely communication with healthcare providers. Telemedicine platforms support remote risk assessments, early interventions, and health education tailored to each pregnancy. Telemedicine is highlighted as a key strategy in Pregnancy care advancements in the US and Tailored Prenatal Care Delivery.
Digital Health Records and Personalized Care Plans
Digital health records enable integrated data management, allowing providers to deliver personalized prenatal care plans that consider medical history, social determinants, and pregnancy progression. These records facilitate shared decision-making by providing clear visualizations of health trends and enabling continuous updates accessible by multidisciplinary care teams. Personalized plans might include customized visit schedules, targeted monitoring strategies, and resource referrals, enhancing overall care quality. This approach aligns with Tailored Prenatal Care Delivery and developing Personalized midwifery care plans.
Improving Access in Underserved Populations
Innovative digital health solutions have become essential in bridging care gaps for marginalized groups who traditionally face challenges like geographic isolation, transportation issues, and systemic biases. By offering telehealth and home monitoring options, pregnant individuals gain easier access to standard prenatal assessments and health education. These technologies have the potential to reduce disparities by supporting early detection of complications and enhancing engagement with healthcare systems. Strategies here resonate with efforts to address Social Determinants of Maternal Health and Improving Maternal and Neonatal Outcomes.
In summary, integrating innovative technologies such as wearable sensors, telemedicine platforms, and digital records is transforming pregnancy care toward a more accessible, personalized, and proactive model that benefits all women, particularly those in underserved communities. This aligns with the Digital transformation of maternity care and the drive for Improving maternal and infant outcomes.
Models of Maternity Care in the United States: Provider Roles and Settings

Hospital births versus home and birth center options
In the United States, the vast majority of births occur in hospitals—approximately 98.4% as of recent data. Hospitals offer comprehensive medical interventions and are equipped to handle complications, making them the predominant choice for maternity care. In contrast, birth centers and home birth options account for a small fraction of deliveries, with birth centers representing roughly 0.52% and home births about 0.99% of all births. These options are primarily available for low-risk pregnancies and are usually attended by midwives or other non-physician providers, appealing to women seeking more natural childbirth experiences or those prioritizing a home-like setting.
Roles of obstetricians, family physicians, certified nurse midwives, and others
Obstetricians and gynecologists are the primary maternity care providers in hospital settings, attending about 90.6% of hospital births. Family physicians also provide obstetrical care, especially in rural communities where physician shortages exist; around 70% of rural women receive obstetrical care from family doctors. Certified Nurse Midwives (CNMs) and other midwives contribute significantly to maternity care, practicing in hospitals, birth centers, and homes. CNMs tend to work predominantly in hospitals and birth centers and provide holistic, family-centered care. Their scope of practice and licensure varies by state, and they are often integrated as part of a collaborative care model along with obstetricians and pediatricians (Maternal and Newborn Care in the United States).
Regionalization of maternity care by facility levels
Maternity care in the U.S. is organized into a regionalized system classified by facility levels from Level I (basic) to Level IV (regional centers offering the highest level of specialized care). This system facilitates the transfer of patients requiring advanced interventions to facilities equipped with appropriate resources and specialists. Regionalization aims to enhance safety and outcomes, ensuring that mothers and newborns with complications receive timely, expert care. It also shapes access, as women in rural or underserved areas might face challenges reaching higher-level centers (Maternity Care in the United States.
Impact on accessibility and care quality
While hospital births with specialized providers ensure a broad range of care options, accessibility issues persist, especially in rural and underserved communities. Provider shortages, particularly of obstetricians and specialists, and geographic barriers affect timely access to care. The presence of family physicians and midwives helps bridge some gaps, yet disparities remain across socioeconomic and racial groups. The diversity in birth settings and provider types contributes to personalized maternity care, but it also requires improved coordination and integration to optimize care quality and equity across the country (Maternal and Newborn Care in the United States.
The Pregnant Workers Fairness Act: Supporting Pregnant Employees’ Health
What is the Pregnant Workers Fairness Act and how does it affect pregnant employees in the US?
The Pregnant Workers Fairness Act (PWFA) is a federal law designed to ensure pregnant employees receive reasonable accommodations in the workplace. It mandates that employers provide these accommodations promptly, without imposing a one-year waiting period. This legal framework makes clear that employers must actively support the health needs of pregnant workers by adjusting work duties or environments to reduce physical strain or stress.
Legal requirements for accommodations
The PWFA requires employers to make necessary accommodations such as modified work schedules, provision of seating, more frequent breaks, or options for lighter duties. Importantly, it acknowledges unpaid leave as a valid accommodation when other adjustments are insufficient. These provisions are designed to safeguard pregnant employees' health and job security simultaneously.
Impact on pregnant workers’ well-being and employment rights
By ensuring access to accommodations, PWFA helps pregnant workers maintain their well-being and employment status. This support can reduce pregnancy-related complications and stress, promoting better maternal and infant health outcomes. Furthermore, the act protects against discrimination and wrongful termination related to pregnancy needs, empowering women to advocate for their health without fear of job loss.
Broader implications for maternal health and workplace support
The PWFA advances the broader goal of integrating maternal health consideration into workplace policies. It complements prenatal care efforts by reducing job-related barriers to health and encouraging workplace environments that prioritize women's health during pregnancy. This holistic approach fosters healthier pregnancies, greater workforce participation among pregnant individuals, and ultimately supports healthier families and communities.
Traditional Prenatal and Postpartum Care Among Diverse Ethnic Communities
Herbal Remedies and Rituals in Different Cultures
Traditional prenatal and postpartum care across diverse ethnic communities often emphasizes the use of herbal remedies in midwifery and culturally significant rituals. For example, in the Kaili ethnic community of Indonesia, herbs like tulasi (holy basil), mugwort, and shallots are incorporated into therapies like herbal steam baths and traditional massage to support maternal well-being. Similarly, Asian cultures use medicinal plants and specific dietary recommendations during pregnancy and the postpartum period to promote healing and prevent illness. These practices are deeply rooted in traditional beliefs in pregnancy, aiming to foster a healthy pregnancy and recovery process.
Umbilical Cord Care and Infant Health Customs
Caring for the newborn's umbilical cord stump involves various cultural methods that reflect ethnic traditions. Customs such as applying salt, boiling the cord, or burying it in specific locations are practiced to protect the infant from infections and spiritual harm. These rituals are intertwined with broader beliefs about the vulnerability of mother and child during the postpartum confinement period found in many Asian and other cultural settings, often described as part of postpartum confinement traditions.
Cultural Significance of Swaddling and Other Infant Care Practices
Swaddling is a widespread practice across multiple ethnic groups, with variations that hold specific cultural meanings and implications for infant health. In some cultures, traditional techniques may include specific patterns of binding or the use of certain textiles. Other infant care traditions include herbal teas for relieving gas pain (using anise, fennel, cumin), natural remedies for diaper rash like olive oil or dry earth application, and practices to promote neonatal beauty or prevent jaundice through culturally symbolic methods. Understanding and practicing safe swaddling and infant care is important to blend cultural childbirth practices with health safety.
Bridging Cultural Practices with Medical Guidance
Modern maternal health care increasingly recognizes the value of integrating traditional wisdom in midwifery with evidence-based medical guidance. Respectful incorporation of cultural practices such as herbal remedies and postpartum rituals alongside scientific prenatal and postnatal care empowers families and improves confidence in health systems. Collaborative approaches involving midwives and healthcare providers who respect cultural customs help bridge traditional care with medical safety and effectiveness, ultimately supporting both maternal and newborn health outcomes.
| Aspect | Examples | Cultural Importance |
|---|---|---|
| Herbal Remedies | Tulasi, mugwort, chamomile | Promote healing and wellness |
| Umbilical Cord Care | Salt application, boiling, burial | Prevent infection and spiritual harm |
| Infant Care Practices | Swaddling, herbal teas for gas, oils | Comfort, health, and cultural identity |
| Integration with Medical Care | Midwife-led culturally sensitive care | Enhance safety, respect, and outcomes |
Preventing Pregnancy: Traditional Natural Family Planning Methods
What are the traditional methods for preventing pregnancy?
Traditional natural family planning methods offer a non-hormonal and holistic approach to pregnancy prevention by leveraging the body's natural reproductive signals and postpartum physiology. Two widely recognized methods are the Fertility Awareness Method (FAM) and the Lactational Amenorrhea Method (LAM).
Fertility Awareness Method (FAM)
The Fertility Awareness Method involves tracking key fertility signs to identify a woman's fertile window during her menstrual cycle. This includes monitoring:
- Menstrual cycle calendar to estimate fertile days
- Basal body temperature changes indicating ovulation
- Cervical mucus consistency and appearance
Couples avoid unprotected sexual intercourse during identified fertile days to prevent conception. With correct and consistent practice, FAM can reach up to 99% effectiveness, although typical use tends to be lower due to the requirement of daily attention and adherence.
Lactational Amenorrhea Method (LAM)
LAM utilizes the natural postpartum infertility that occurs when a woman exclusively breastfeeds her infant. Exclusive breastfeeding suppresses ovulation, providing a natural contraceptive effect for up to six months postpartum, as long as the mother has not resumed menstruation. LAM effectiveness exceeds 99% in this period when practiced correctly.
Effectiveness and Limitations
While these methods can be highly effective when correctly applied, they require dedication, education, and often professional guidance to ensure accurate identification of fertile periods or adherence to breastfeeding patterns. Limitations include:
- No protection against sexually transmitted infections (STIs)
- Reduced effectiveness with inconsistent practice or early return of ovulation
- Necessity for motivated users to maintain strict observation
Integration with Modern Contraceptive Counseling
Healthcare providers often integrate traditional natural family planning within broader contraceptive counseling. By educating women about the advantages and limitations of these methods alongside modern options, providers empower women to make informed reproductive choices. Combining natural methods with barrier protections like condoms can enhance safety by offering STI prevention. Personalized counseling and follow-up support improve success rates and user satisfaction.
Natural family planning respects women's desire for holistic, culturally sensitive approaches to pregnancy prevention, aligning with comprehensive maternal and infant care.
Respectful Maternity Care: Combating Disrespect and Abuse During Childbirth

Prevalence and impact of disrespect and abuse (D&A)
Disrespect and abuse during childbirth remain significant global issues, with studies reporting a prevalence as high as 62.5% in some settings, such as a study in Saudi Arabia. Non-consented care is the most common form encountered. Such negative experiences can severely erode maternal trust in healthcare systems, cause emotional distress, and deter women from seeking institutional childbirth in the future.
The IDEAL approach to improve maternity care culture
To address these challenges, the IDEAL approach has been recommended. This strategy encompasses several components:
- Intervention to prevent mistreatment: Implementing policies and protocols to eliminate disrespectful behaviors.
- Devising monitoring tools and audit policies: Regular assessments to identify and address instances of D&A.
- Allowing companionship during labor: Encouraging the presence of support persons to enhance emotional comfort.
- Training healthcare staff in stress-coping and respectful care: Building providers' capacity for empathetic, patient-centered care.
Ensuring dignity, consent, and respectful treatment
Every woman has the right to dignified, respectful care throughout pregnancy and childbirth. This includes obtaining informed consent for all procedures, providing clear communication, and upholding privacy and autonomy. Reducing the number of caregivers present during labor and cautiously managing delivery methods can also decrease the likelihood of disrespectful experiences.
Improving trust and engagement in institutional childbirth settings
Building trust requires fostering respectful, culturally sensitive care environments. Training staff in communication and empathy, integrating patient preferences through shared decision-making, and involving multidisciplinary teams can enhance maternal satisfaction and outcomes. Ultimately, the goal is a maternity care culture where all women feel safe, empowered, and supported, promoting positive health behaviors and improved maternal and neonatal health.
Collaborative Care Models: Enhancing Support Networks for Mothers
How do midwives, obstetricians, pediatricians, lactation consultants, and mental health professionals collaborate in maternal care?
Collaborative care models in maternity care bring together a range of healthcare professionals including midwives, obstetricians, pediatricians, lactation consultants, and mental health experts. This multidisciplinary approach ensures comprehensive maternal and infant care for both mother and infant. Each specialist contributes their expertise to assess physical health, support breastfeeding, monitor infant development, and address emotional well-being. For instance, modern midwifery emphasizes holistic support and personalized care, obstetricians manage complex pregnancies and medical interventions, pediatricians oversee newborn health, while lactation consultants provide breastfeeding guidance. Mental health professionals focus on maternal psychological health, screening for perinatal depression and anxiety, which promotes positive long-term outcomes.
What is the role of doulas and family support in enhancing maternity care?
Doulas and family members form an essential support network during pregnancy, labor, and the postpartum period. Doulas provide continuous childbirth support, emotional encouragement, and advocacy, which enhances maternal satisfaction and lowers intervention rates. Family involvement complements professional care by providing practical assistance, emotional reassurance, and culturally sensitive support. Together, they foster a nurturing environment that empowers women in decision-making, reduces stress, and improves bonding with their newborns.
How does comprehensive and continuous maternal and infant care improve health outcomes?
Continuous support before, during, and after childbirth allows for early identification and management of health issues, nutritional guidance, breastfeeding support, and mental health care. Individualized care plans developed through Tailored Prenatal Care Delivery help tailor services to each woman's unique needs, increasing adherence and satisfaction. Group prenatal care models and telemedicine are effective strategies that enhance accessibility and promote engagement. These approaches contribute to reduced rates of preterm birth, low birth weight, and postpartum depression, while improving breastfeeding initiation and duration.
What are the benefits of collaborative care on maternal satisfaction?
Women receiving multidisciplinary, continuous support report feeling more confident, informed, and prepared for childbirth and parenting. Collaboration facilitates respectful, culturally sensitive care and empowers women to actively participate in their pregnancy and birth plans. The integration of traditional wisdom and evidence-based care, supported by multidisciplinary teams, results in a more patient-centered experience that is associated with better maternal and infant health outcomes.
| Aspect | Description | Benefit |
|---|---|---|
| Multidisciplinary teams | Midwives, obstetricians, pediatricians, lactation consultants, mental health professionals | Comprehensive care addressing physical, emotional needs |
| Doulas & family support | Continuous labor and emotional support | Enhanced satisfaction, reduced stress, empowered decisions |
| Continuous care | Support throughout pregnancy, birth, postpartum | Improved health outcomes, earlier detection of complications |
| Tailored plans | Shared decision-making and personalized care | Greater patient engagement and improved adherence |
Future Directions: Innovations and Policy for Improved Pregnancy Care

Expanding Access to Care via Telehealth and Community Programs
Telehealth has become a pivotal innovation in maternity care, especially highlighted during the COVID-19 pandemic. It enables flexible and individualized prenatal care by offering remote consultations, telemonitoring, and virtual group prenatal sessions. This Digital transformation of maternity care helps overcome barriers such as transportation, work commitments, and geographic isolation, particularly in underserved areas. In tandem, community programs incorporating doulas, midwives, and home visiting services strengthen local support networks, addressing social determinants that impact maternal health outcomes.
Policy Initiatives to Reduce Maternal Mortality and Disparities
Efforts to reduce maternal mortality in the United States and globally emphasize addressing systemic inequities. Policies focus on expanding Medicaid coverage, supporting implicit bias training for care providers, and increasing access to culturally competent care. State-level programs are adopting data-driven strategies including perinatal quality collaboratives and implicit bias interventions. These initiatives target disparities disproportionately affecting marginalized racial and socioeconomic groups by improving early prenatal engagement, enhancing mental health screening, and facilitating referrals for unmet social needs (Maternity Care in the United States, prenatal care importance).
Sustainability of Group Prenatal Care and Enhanced Antenatal Care Models
Group prenatal care models like CenteringPregnancy model have demonstrated success in improving birth outcomes, patient satisfaction, and reducing costs by fostering peer support and education. However, challenges such as resource allocation, leadership changes, and reimbursement policies limit wide adoption. Enhanced Antenatal Care blends individualized and group approaches to reduce fear of childbirth and increase knowledge about postpartum care. Sustaining these models requires organizational commitment, adequate space and staff, and systemic adjustments to funding mechanisms (Enhanced Antenatal Care (EAC)).
Leveraging Traditional Knowledge and Technology for Next-Generation Maternity Care
Integrating ancestral and cultural practices with evidence-based medical care presents a promising frontier. Traditional midwives in Latin America use herbal remedies, massage, and spiritual support alongside biomedical tools, enhancing maternal and neonatal outcomes, especially in rural and indigenous communities. Simultaneously, advanced technologies such as digital health records, remote monitoring devices, and stem cell banking (e.g., Cord blood) enhance personalized care (Holistic approaches to pregnancy, Femtech revolution in pregnancy care). This blended approach respects cultural safety and harnesses innovation for comprehensive maternity care.
The future of pregnancy care hinges on the synergy of technological advancements, policy reform, culturally informed practices, and sustainable care models—all aimed at improving equity, safety, and experience for mothers and their infants.
Towards Integrated Pregnancy Care: Respecting Heritage, Embracing Innovation
Combining Traditional Wisdom with Modern Science for Optimal Care
Integrating traditional pregnancy and childbirth practices with evidence-based medical care offers comprehensive benefits to mothers and infants. Traditional approaches, such as herbal remedies, massage, and cultural postpartum rituals, provide emotional comfort and foster community support. When combined with modern advances—including continuous monitoring, personalized care plans, and emerging technologies like telemedicine—this blended model enhances safety, improves health outcomes, and promotes holistic well-being.
Embracing Culturally Sensitive, Patient-Centered Care
Respecting cultural beliefs and traditional practices is essential to build trust and engagement in maternity care. Patient-centered models encourage shared decision-making and personalized visit schedules that honor individual preferences and social contexts. Providing education that empowers women, offering support from culturally-aware providers such as midwives and doulas, and facilitating community-based care help reduce disparities. Such approaches acknowledge the physical, emotional, and spiritual needs of women, promoting better maternal satisfaction and outcomes.
Advancing Innovation and Equity in Maternal Health
Ongoing innovation is crucial in addressing systemic barriers and expanding access to quality maternity services. Flexible care options including group prenatal care, telehealth, and integrated care teams support diverse populations effectively. Healthcare systems must prioritize equity to overcome disparities linked to race, socioeconomic status, and geography. Through collaboration among providers, including traditional midwives and biomedical professionals, and commitment to respectful treatment, maternity care can evolve to be inclusive, effective, and empowering for all women and families.



.png)